SECOND OPINION SERIES
Natural Treatment for OCD Symptoms | Understanding Glutamate, NMDAR & Biochemical Patterns
A comprehensive natural treatment plan for OCD symptoms begins with understanding how diet for OCD symptoms, supplements for OCD symptoms, and recommended lab tests for OCD work together to regulate glutamate, methylation, and NMDA receptor activity. Many patients notice that intrusive thoughts, agitation, or sensory overload intensify after certain foods or during periods of inflammation, and these patterns often reveal measurable biochemical imbalances. By combining targeted nutritional strategies, carefully selected supplements, and lab testing that identifies undermethylation, copper/zinc imbalance, or oxidative stress, patients can dramatically reduce the excitatory pressure that drives looping thoughts and internal tension.
In the Second Opinion Series, I explain how these biochemical patterns create the “overactive OCD brain” and how a natural therapy for OCD symptoms can target glutamate, NMDAR, and methylation instead of relying only on serotonin medications.
Near the top of this article, we’ll keep things patient-friendly and practical. Later, you’ll find a deeper scientific section for readers who want the neurochemistry behind glutamate and OCD symptoms explained in detail.

Natural Treatment for OCD Symptoms: How Glutamate and NMDAR Drive Intrusive Thoughts
A natural treatment for OCD symptoms must focus on calming glutamate, reducing NMDAR overactivity, and supporting methylation, zinc balance, and antioxidant capacity. Many patients seeking a natural treatment for OCD symptoms experience looping thoughts, intrusive images, and internal pressure because their neurobiology is excessively excitatory—not because of weak willpower. A natural treatment for OCD symptoms addresses biochemical overload by lowering glutamate, reducing excitotoxic signaling, and stabilizing inhibitory pathways such as GABA and serotonin. When these biochemical levers are corrected, a natural treatment for OCD symptoms often produces clearer thinking, fewer intrusions, and more emotional resilience.
From a clinical perspective, a natural treatment for OCD symptoms aims to quiet excessive glutamate, stabilize NMDAR activity, strengthen inhibitory pathways (GABA, serotonin), and address methylation or copper/zinc imbalances. The goal is not to “turn off” thinking, but to reduce the biochemical pressure that makes thoughts feel intrusive and uncontrollable.
Patients describe this pattern as:
-
“My brain won’t stop scanning for problems.”
-
“It feels like static or electrical pressure in my head.”
-
“Even when I know the thoughts aren’t rational, they won’t let go.”
These experiences are not character flaws. They are evidence of specific biochemical patterns that can be measured and treated.
Glutamate and OCD Symptoms Explained: Why Excitatory Signaling Fuels Looping Thoughts
Glutamate and OCD symptoms explained in simple terms: glutamate is the brain’s primary “go” signal. It powers focus, learning, and memory—but too much glutamate, in the wrong places, turns circuits into rigid loops instead of flexible networks.
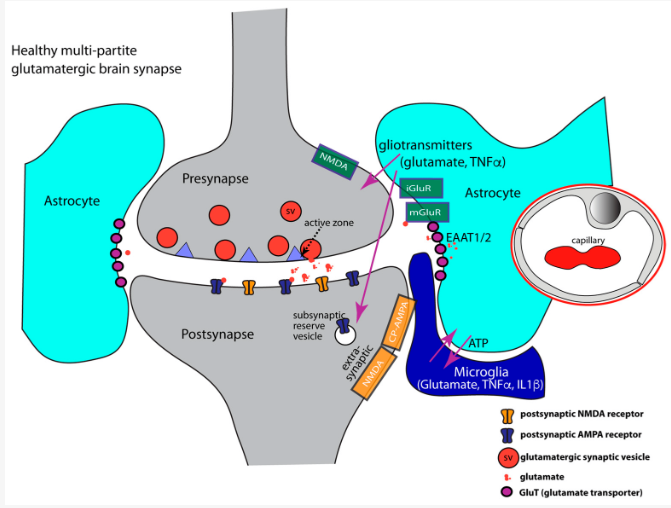
In OCD, elevated extracellular glutamate overstimulates the cortico-striato-thalamo-cortical (CSTC) loop—the network responsible for error detection and habit formation. When that loop fires too often, the brain keeps sending “something’s wrong” signals, even when nothing is actually wrong.
Mechanisms:
-
Elevated glutamate between neurons overstimulates circuits that drive intrusive thoughts and compulsions.
-
Underactive EAAT transporters (glutamate reuptake) slow clearance of glutamate from synapses.
-
Neuroinflammation and microglial activation increase glutamate release under stress or infection.
-
Low zinc and high copper remove natural brakes on glutamate and NMDAR activity.
-
Oxidative stress destabilizes glutamate–GABA balance, increasing “noise” and mental static.
When you feel OCD symptoms spike for no obvious psychological reason, this glutamate-driven physiology is often the missing explanation.
NMDAR and OCD Symptoms Explained: The Receptor That Controls Intrusive Thought Intensity
To understand NMDAR and OCD symptoms explained, think of the NMDA receptor as a “gain control” knob on excitatory signaling. NMDARs respond to glutamate and allow calcium into neurons, which is necessary for learning and memory. But if this receptor is overactive, circuits become hyper-reactive, rigid, and difficult to shut down.
In OCD, NMDAR overactivity:
-
Increases the intensity of intrusive thoughts and mental images.
-
Makes the CSTC loop “stickier”—obsessions feel more compelling and urgent.
-
Contributes to insomnia, sensory overload, and internal pressure.
When NMDARs fire too often:
-
Calcium influx triggers intracellular stress and excitotoxicity.
-
Glycine and D-serine co-activation can further sensitize the receptor.
-
Low GABA and low zinc remove normal inhibitory control.
-
High copper indirectly amplifies NMDAR activity by weakening GABAergic tone.
This is why many patients feel that standard SSRIs only partly help, or help at first and then flatten out. The core issue isn’t always serotonin—it is glutamate/NMDAR overdrive.
Undermethylation and Natural Treatment for OCD Symptoms
Undermethylation is one of the most consistent Walsh-style patterns in OCD. Low SAMe, elevated histamine, lower serotonin tone, and impaired antioxidant capacity all predispose the brain to excitatory overload. When undermethylation is present, a natural treatment for OCD symptoms must also address methylation—not just glutamate.
Typical undermethylator features:
-
Inner tension, perfectionism, and strong sense of responsibility
-
Seasonal depression, ritualized thinking, or rigid moral code
-
High histamine, elevated homocysteine, or low SAM/SAH ratio on labs
Mechanisms:
-
Low SAMe impairs regulation of genes and enzymes that control neurotransmitter turnover.
-
High histamine reflects global undermethylation and increases neural reactivity.
-
Reduced glutathione weakens antioxidant defenses, increasing oxidative triggers.
-
Low B6/P5P slows conversion of glutamate → GABA, worsening excitatory dominance.
For these patients, a natural therapy for OCD symptoms often includes methylation support, zinc, B6, magnesium, and antioxidant strategies alongside glutamate-targeted interventions.
Inflammation, Microglia, and Glutamate in OCD Symptoms
A growing literature links OCD with low-grade neuroinflammation—especially in PANS/PANDAS, mold exposure, chronic infections, or trauma-related physiology. Microglia (the brain’s immune cells) release glutamate and cytokines when activated, which can directly worsen glutamate and OCD symptoms.
Key points:
-
IL-6 and TNF-α increase NMDAR phosphorylation and sensitivity.
-
Blood–brain barrier permeability rises with chronic inflammation, making neurons easier to overstimulate.
-
Oxidative stress prolongs glutamate signaling and destabilizes mitochondrial energy production.
Clinically, this looks like OCD flares when the immune system is provoked—after illness, exposures, major stress, or sleep loss. Anti-inflammatory strategies are therefore part of many natural therapies for OCD symptoms, particularly in complex cases.
Ketogenic Therapy as a Natural Treatment for OCD Symptoms
Ketogenic strategies—whether diet or ketone esters—can function as a powerful natural treatment for OCD symptoms because ketones calm excitatory signaling, increase GABA tone, and stabilize mitochondria.
Mechanisms:
-
Ketones reduce NMDAR hyperactivity, lowering excitatory pressure.
-
β-hydroxybutyrate increases GABA production, improving inhibitory balance.
-
Improved ATP output enhances cognitive endurance and emotional resilience.
-
Reduced oxidative stress and inflammation normalize glutamate clearance and EAAT function.
For patients with severe glutamate/NMDAR-driven OCD, ketone esters or carefully supervised ketogenic diets can be an important adjunct to Walsh-style nutrient therapy. They do not replace methylation work; they lower the background noise so other interventions can work better.
Walsh Protocol and Best Supplements for OCD Symptoms
Recommended lab tests for OCD are essential for identifying the biochemical patterns that drive intrusive thoughts and compulsive behaviors. These recommended lab tests for OCD clarify whether undermethylation, copper imbalance, oxidative stress, mitochondrial strain, or glutamate excess is contributing to symptoms. Because OCD is highly biochemical rather than purely psychological, recommended lab tests for OCD help determine which nutrients, methylation supports, and antioxidant strategies will be most effective. Patients who complete recommended lab tests for OCD consistently gain clarity about why their symptoms fluctuate and how to target treatment properly.
Core Walsh-compatible targets:
-
Zinc – dampens NMDAR activity, supports GABA receptors, lowers free copper.
-
B6 / P5P – helps convert glutamate into GABA; stabilizes neurotransmitter synthesis.
-
Methionine / SAMe precursors – support undermethylation without overshooting.
-
Magnesium (especially glycinate or threonate) – natural NMDAR blocker, calms neuronal firing.
-
Antioxidants (vitamin C, NAC, E, selenium) – reduce oxidative stress that drives NMDAR sensitivity.
-
Copper-normalizing strategies – zinc, protein support for ceruloplasmin, and hormonal assessment.
When we talk about the best supplements for OCD symptoms, the goal is not a random list of “calming” products. It’s a targeted set of nutrients based on the patient’s biotype and lab data.
Foods and Glutamates: How Diet Influences OCD Symptoms Through NMDAR Sensitivity
A diet for OCD symptoms must lower free glutamate, reduce histamine load, support zinc status, and stabilize blood sugar to prevent NMDAR overactivity. Many patients notice that a diet for OCD symptoms greatly reduces intrusive thoughts because it removes food-based triggers that elevate glutamate or inflammatory signaling. The most effective diet for OCD symptoms avoids MSG, processed foods, fermented products, and aged cheeses, while emphasizing zinc-rich proteins, magnesium-rich vegetables, and anti-inflammatory fats. When applied consistently, a diet for OCD symptoms can dramatically reduce mental agitation, sensory overload, and obsessive looping.
Many people notice that OCD flares after restaurant meals, processed foods, or certain “comfort” foods. That pattern is biochemical, not imagined.
High-Glutamate Foods That May Worsen OCD Symptoms
Free glutamate (unbound and rapidly absorbed) is most problematic in individuals with glutamate-sensitive OCD or undermethylation.
Common culprits:
-
MSG and hidden glutamate (yeast extract, “natural flavors,” hydrolyzed proteins)
-
Soy sauce, miso, and other fermented soy products
-
Bone broth / long-simmered broths (especially 8+ hours)
-
Parmesan and aged cheeses
-
Tomato paste, sauces, and concentrates
-
Mushrooms, cured meats, and ultra-processed snacks
In patients with high histamine, zinc deficiency, or copper overload, these foods can sharply increase intrusive thoughts, insomnia, or internal agitation.
Histamine, Copper/Zinc, and OCR Symptom Intensification
Histamine is cleared by methylation. In undermethylated OCD patients, high-histamine foods (fermented foods, cured meats, alcohol, leftovers) add a second layer of stress. Copper-heavy diets (chocolate, nuts, seeds, shellfish, certain greens) become problematic when zinc is low.
Net effect:
-
Higher histamine → more neural reactivity
-
Higher effective copper → more norepinephrine and glutamate tone
-
More NMDAR sensitivity → intensified OCD loops
This is why dietary response frequently predicts biotype long before labs return.
Calming Foods for Glutamate-Sensitive OCD
Supportive dietary patterns emphasize:
-
Zinc-rich animal protein (oysters, beef, lamb, poultry)
-
Eggs and clean fats (avocado, olives, olive oil)
-
Magnesium-rich greens and seeds (in tolerated amounts)
-
Omega-3–rich fish (salmon, sardines)
-
Low-glutamate vegetables (cucumber, lettuce, carrots, squash)
-
Herbal teas (chamomile, lemon balm) that reduce excitatory tone
Diet is not a cure, but for many it is a powerful part of a natural therapy for OCD symptoms.
Best Supplements for OCD Symptoms: NAC, Magnesium, Zinc, and More
The best supplements for OCD symptoms are those that regulate glutamate, reduce NMDAR hyperactivity, support methylation, and correct copper/zinc imbalance. For most patients, the best supplements for OCD symptoms work because they directly influence excitatory pressure that drives intrusive thoughts and compulsive behaviors. Rather than offering general “calming agents,” the best supplements for OCD symptoms target the biochemical pathways—glutamate overload, oxidative stress, undermethylation, and zinc deficiency—that intensify OCD loops. When chosen correctly, the best supplements for OCD symptoms can significantly improve cognitive flexibility and emotional stability.
Key options:
-
N-Acetylcysteine (NAC)
-
Modulates glutamate via the cystine–glutamate exchanger
-
Raises glutathione, protecting against NMDAR-driven oxidative stress
-
Supports homocysteine metabolism, easing SAH-related methylation bottlenecks
-
-
Magnesium (glycinate or threonate)
-
Acts as a physiologic NMDAR blocker
-
Reduces neural hyperexcitability and improves sleep
-
-
Zinc
-
Antagonizes NMDAR activity
-
Stabilizes GABA function and reduces free copper
-
-
B6 / P5P
-
Helps convert glutamate into GABA
-
Essential for Walsh-style protocols in undermethylation and pyroluria
-
-
Creatine (in undermethylation)
-
Reduces methylation demand by lowering endogenous creatine synthesis
-
Frees SAMe for neurotransmitter and DNA methylation, indirectly calming excitatory tone
-
-
Ketogenic or ketone ester strategies
-
Decrease glutamate activity, increase GABA, and stabilize mitochondrial function
-
This is what I mean by recommended supplements for OCD symptoms: individually chosen, biochemically justified, and integrated with lab data.
Recommended Lab Tests for OCD and Biochemical Pattern Detection
For many patients, the most empowering step is to run recommended lab tests for OCD that clarify what’s happening biochemically—not just neurologically.
Primary lab tests for OCD symptoms in my practice:
-
Walsh Panel
-
Whole blood histamine (undermethylation marker)
-
Plasma zinc, serum copper, ceruloplasmin, zinc:copper ratio
-
Pyrrole testing for pyroluria (zinc/B6 wastage)
-
-
Doctor’s Data Methylation Pathways Panel
-
SAM, SAH, homocysteine, methionine
-
SAM/SAH ratio (methylation efficiency)
-
Patterns that show if methylation is overworked or under-powered
-
-
Organic Acids
-
Mitochondrial strain, oxidative stress, and sometimes glutamate-related metabolites
-
-
Basic metabolic and inflammatory markers
-
Vitamin D, B12, folate, CRP, fasting glucose, and HbA1c
-
These recommended lab tests for OCD don’t diagnose OCD itself—they explain why some patients have intense glutamate/NMDAR-driven symptoms and why a natural treatment for OCD symptoms may be highly effective.
Diet for OCD Symptoms | Glutamates, NMDA Receptors, Histamine & Copper/Zinc Balance
A strategic diet for OCD symptoms aims to reduce free glutamate, stabilize histamine levels, support zinc balance, and lower inflammation—all of which influence NMDA receptor sensitivity. Many patients report that intrusive thoughts or agitation worsen after certain meals, and this pattern often reflects how food choices affect glutamate signaling and methylation stress. By identifying personal triggers and emphasizing nutrient-dense, low-glutamate foods, a diet for OCD symptoms can meaningfully reduce internal tension, sensory overload, and cognitive looping without feeling restrictive.
This section explains the diet for OCD symptoms based on glutamate physiology and Walsh biotypes. It also includes the foods that worsen NMDAR overactivity—and the foods that calm it.
How Diet Influences Glutamate and OCD Symptoms
A proper diet for OCD symptoms aims to reduce excessive glutamate signaling while supporting zinc, methylation, mitochondrial function, and antioxidant pathways. Many patients notice:
-
intrusive thoughts worsen after certain foods
-
insomnia or agitation after restaurant meals
-
more compulsive urges after processed foods or glutamate-rich snacks
This is not psychological. It is glutamate and NMDAR physiology, magnified by stress, inflammation, or undermethylation.
Mechanisms behind diet-triggered OCD flares:
-
Free glutamate from foods binds directly to glutamate receptors.
-
High-histamine foods overwhelm undermethylated individuals, raising neural reactivity.
-
High-copper foods intensify norepinephrine and glutamate tone.
-
Inflammatory meals activate microglia, which release glutamate.
-
Low-zinc diets remove a natural brake on NMDA receptor activation.
If you have glutamate-sensitive OCD, you FEEL your diet because your receptors respond quickly.
Best Supplements for OCD Symptoms
When determining the best supplements for OCD symptoms, the goal is to reduce excitatory pressure and restore neurochemical regulation. These are the most consistent clinical tools:
N-Acetylcysteine (NAC)
• reduces glutamate buildup through the cystine-glutamate exchanger
• improves antioxidant capacity
• decreases oxidative stress driving NMDA hyperactivity
Magnesium (glycinate or threonate)
• natural NMDA receptor blocker
• calms neuronal firing
• improves sleep and reduces sensory overload
Glycine
• co-agonist that stabilizes NMDA receptor kinetics
• reduces the “over-reactive” quality of the receptor
Creatine (Walsh-compatible when undermethylation present)
• reduces methylation strain
• stabilizes brain energy systems that regulate inhibitory tone
Zinc
• antagonizes NMDA receptors
• improves GABA activity
• foundational in undermethylation and copper imbalance
Ketogenic strategies (diet or ketone esters)
• reduce glutamate activity
• increase GABA
• stabilize mitochondria
• lower neuroinflammation
These form the foundation of best supplements for OCD symptoms within biochemical and functional treatment models.
FAQ's - Natural Treatment for OCD Symptoms
2. Can supplements really help OCD symptoms?
Yes—supplements can be effective for OCD symptoms when they address the underlying biochemical patterns like undermethylation, high glutamate, or copper overload. When chosen correctly, they stabilize neurotransmitters and reduce the internal pressure that drives obsessions and compulsions. Clinical results are strongest when supplements are guided by lab testing rather than guesswork.
3. How does glutamate contribute to OCD symptoms?
Excess glutamate overstimulates brain circuits involved in intrusive thoughts and repetitive behaviors. When glutamate clearance is impaired or NMDA receptors are too sensitive, the brain gets stuck in “overdrive,” producing the characteristic OCD cycle. Reducing glutamate activity through nutrients, diet, and metabolic therapies can significantly improve symptoms.
4. What is the connection between NMDAR and OCD symptoms?
NMDARs are glutamate-sensitive receptors that regulate learning, memory, and behavioral precision. When NMDAR activity becomes excessive—often due to stress, inflammation, undermethylation, or low zinc—the brain becomes rigid, anxious, and unable to shut off intrusive thoughts. Understanding NMDAR overstimulation helps explain why some individuals do not improve on typical psychiatric medications.
5. What lab tests are recommended for OCD symptoms?
The most useful lab tests for OCD symptoms include whole blood histamine, SAM/SAH methylation status, plasma zinc, serum copper, ceruloplasmin, and B6/P5P levels. These tests reveal whether undermethylation, oxidative stress, or copper-driven glutamate excess is contributing to symptoms. Testing helps create a more accurate and effective natural treatment plan.
6. How does undermethylation make OCD symptoms worse?
Undermethylation reduces SAMe availability, increases histamine, weakens inhibitory pathways, and exaggerates glutamate-driven excitatory activity. This heightens internal tension, perfectionism, compulsive thinking, and emotional rigidity. Supporting methylation often brings significant relief because it stabilizes neurotransmitter pathways involved in OCD.
7. Why do some people with OCD not respond well to SSRIs?
SSRIs increase serotonin but do not address glutamate excess, NMDAR hyperactivity, or methylation problems—three of the most common biochemical patterns in OCD. For undermethylators, serotonin-based medications can even worsen emotional tension or create emotional flattening. Natural treatments target the root neurochemical drivers rather than relying solely on serotonin modulation.
8. Can ketogenic or metabolic therapy help OCD symptoms?
Yes—therapeutic ketosis can stabilize glutamate-GABA balance, reduce NMDAR activity, and improve cognitive flexibility. Ketones act as a clean fuel for the brain, lowering inflammation and reducing the intensity of intrusive thoughts. Many patients notice improvements in sleep, mood stability, and compulsive urges when achieving stable therapeutic ketosis.
9. Does copper imbalance contribute to OCD symptoms?
High free copper increases norepinephrine, weakens GABA function, and amplifies glutamate signaling—all of which intensify OCD symptoms. Many cases of anxiety-heavy or agitation-heavy OCD improve once zinc is restored and copper is brought back into balance. Testing copper, zinc, and ceruloplasmin is essential for anyone with fluctuating or hormone-sensitive OCD symptoms.
10. How long does it take for natural treatments to help OCD?
Most people begin noticing changes within 4–8 weeks once methylation is supported and glutamate/NMDAR regulation improves. More significant improvements—especially in intrusive thought frequency and compulsive behaviors—often appear over 12–16 weeks as brain chemistry stabilizes. Lab-guided treatment accelerates results and reduces trial-and-error.
Scientific Section: Glutamate, NMDAR Activity, and Biochemical Drivers of OCD Symptoms
Obsessive–compulsive disorder is widely recognized for its pattern of intrusive thoughts and repetitive behaviors, but the biological roots extend far beyond serotonin. Modern neuroimaging, cerebrospinal fluid studies, and postmortem analyses consistently show glutamatergic dysregulation in individuals with OCD. Glutamate is the brain’s primary excitatory neurotransmitter, and when its activity becomes excessive—or poorly regulated—the neural circuits that govern behavioral inhibition and cognitive flexibility become overactive.
Central to this process is the cortico-striato-thalamo-cortical (CSTC) loop, the network responsible for error detection, habit formation, and behavioral gating. Hyperactivity in this loop produces the classic OCD cycle: perceived error → intrusive thought → compulsive behavior → temporary relief → rapid return of error signals. Much of this hyperactivity is driven by altered NMDA receptor (NMDAR) activity, which amplifies excitatory signaling and prevents the brain from “resetting” intrusive cognitive sequences.
Why NMDAR Hyperactivity Matters in OCD
-
Elevated glutamate concentrations overstimulate NMDAR channels.
-
Excessive calcium influx increases intracellular stress and metabolic strain.
-
Overactive NMDAR signaling potentiates the CSTC loop, reinforcing intrusive thoughts and rituals.
-
Zinc deficiency, copper imbalance, inflammation, and undermethylation all sensitize NMDARs.
-
When inhibitory GABA signals are low, excitatory circuits dominate unopposed.
These mechanisms explain why OCD symptoms often worsen under physiological stress, hormonal fluctuations, sleep deprivation, or nutritional imbalance—and why conventional serotonin-based therapies may fail.
NMDAR Excitotoxicity and Its Emotional, Cognitive, and Physical Symptoms
Although “excitotoxicity” is a term usually applied to neurodegenerative disease, milder forms of NMDAR-driven hyperexcitability are increasingly recognized in psychiatric conditions, including OCD, anxiety, and trauma-related disorders. When NMDARs are overstimulated, they allow excess calcium into neurons, activating enzymatic pathways that disturb energy metabolism, damage membranes, alter synaptic proteins, and destabilize neurotransmission.
Physical manifestations
-
Seizure tendency or subclinical motor overactivation
-
Muscle rigidity, spasms, or somatic tension
-
Migraines, head pressure, or sensory amplification
-
Autonomic disruption—racing heart, heat intolerance, nausea
-
Visual or auditory distortions in severe cases
Emotional and cognitive manifestations
-
Heightened anxiety not responsive to standard anxiolytics
-
Racing thoughts, mental “pressure,” or cognitive looping
-
Irritability, sensory defensiveness, and emotional reactivity
-
Intrusive imagery, intrusive fear-based thoughts
-
Memory instability, slowed processing, or reduced cognitive flexibility
-
Sleep disruption from persistent neural hyperarousal
This symptom constellation frequently overlaps with high copper, zinc deficiency, undermethylation, neuroinflammation, and pyroluria—core biochemical drivers in the Walsh model.
Mechanisms Relevant to Natural OCD Treatment
1. Glutamate Dysregulation in OCD: What the Research Shows
Studies consistently find elevated glutamate in the anterior cingulate cortex and basal ganglia of individuals with OCD. These regions govern error detection, habit formation, and cognitive switching. Excess glutamate amplifies neural firing in the CSTC loop, making it difficult to disengage from intrusive thoughts or repetitive actions.
Key scientific points
-
Magnetic resonance spectroscopy (MRS) shows elevated glutamate in OCD subtypes.
-
Glutamate increases intracellular calcium and energy demand.
-
Hyperactivity in CSTC loops correlates with symptom severity.
-
Zinc deficiency worsens glutamate release and NMDAR sensitivity.
-
Elevated homocysteine and SAH reinforce excitatory tone.
2. NAC (N-Acetylcysteine): Glutamate Modulation and Antioxidant Stabilization
NAC’s therapeutic effect in OCD is not simply due to antioxidant activity. NAC modulates glutamate through the cystine–glutamate antiporter (system xc−), helping reduce synaptic glutamate overflow and stabilizing NMDAR activity. NAC also enhances glutathione synthesis, protecting neurons from excitatory stress.
Mechanisms of NAC relevant to OCD
-
Regulates glutamate release and reuptake, reducing excitotoxic signaling.
-
Boosts glutathione, countering oxidative stress and inflammatory triggers.
-
Lowers homocysteine, reducing SAH accumulation and improving methylation kinetics.
-
Supports Walsh-style nutrient protocols, particularly when histamine is high.
-
Stabilizes NMDAR activity, reducing intrusive thought spirals.
NAC is one of the few nutraceuticals with published randomized controlled trials showing clinical benefit in OCD and related compulsive-spectrum disorders.
3. Undermethylation and OCD: Why It Amplifies Glutamate Circuits
Undermethylation reduces SAMe availability, slows histamine clearance, increases oxidative stress, and desensitizes inhibitory neurotransmission. Low SAMe also leads to elevated SAH, which inhibits methyltransferases and destabilizes neurotransmitter metabolism. This produces a neurochemical environment in which NMDAR hyperactivity is more likely.
Why undermethylation intensifies OCD symptoms
-
Reduced SAMe → impaired synthesis of serotonin, dopamine, and phospholipids
-
Elevated histamine → increased neural reactivity and obsessive focus
-
Low glutathione → reduced buffering of excitatory stress
-
Increased SAH → impaired regulation of NMDAR and COMT
-
Higher oxidative stress → increased intrusive cognitive activity
This explains why undermethylators are prone to OCD, perfectionism, ritualistic thinking, and inner tension.
4. Ketamine in Low Doses: NMDAR Reset, Synaptic Plasticity, and Rapid Circuit Stabilization
At subanesthetic doses, ketamine acts selectively on NMDAR channels, reducing pathological excitatory signaling in the CSTC loop without producing full dissociation. Ketamine also enhances AMPA receptor throughput, increases BDNF, and promotes rapid synaptogenesis—effects that allow the brain to break out of entrenched obsessive cognitive cycles.
Mechanisms relevant to OCD physiology
-
NMDAR blockade reduces immediate excitatory overdrive.
-
AMPA activation improves cortical flexibility and mood stability.
-
BDNF upregulation enhances synaptic repair and circuit normalization.
-
Neuroinflammation reduction helps restore normal neurotransmission.
-
Interrupts CSTC loop hyperactivity, lowering obsessional intensity.
Although not part of Walsh Protocol, ketamine’s physiology aligns with the goals of reducing glutamate-driven rigidity and improving circuit adaptability.
5. How These Mechanisms Integrate Within the Walsh Model
OCD commonly arises from a biochemical constellation rather than a single neurotransmitter defect:
-
High glutamate + NMDAR hyperactivity
-
Histamine elevation + undermethylation
-
Low zinc + high copper → increased excitatory tone
-
Oxidative stress + reduced glutathione
-
Impaired inhibitory (GABA) activity
NAC, zinc, magnesium, methylation support, copper regulation, antioxidants, and sometimes low-dose ketamine synergistically improve glutamate balance, methylation capacity, and neuroplasticity—the true levers in OCD physiology.



