Decoding Homocysteine's Role in Heart Health
Cardiovascular disease remains a leading cause of death worldwide, and understanding the factors that contribute to its development is essential for prevention and treatment. For years, cholesterol has been considered the gold standard for determining cardiovascular risk, leading to dietary recommendations that restrict exogenous sources of cholesterol. However, recent research has shifted the focus to the roles of homocysteine, inflammation, and oxidative stress in cardiovascular health. This comprehensive post will explore the complex relationship between homocysteine, cholesterol, and cardiovascular risk, and provide insights on how to manage risk through diet, lifestyle, and supplementation.
I. Lower Homocysteine Levels: Understanding Homocysteine and Cholesterol
A. Homocysteine's Impact on Cardiovascular Health and Beyond
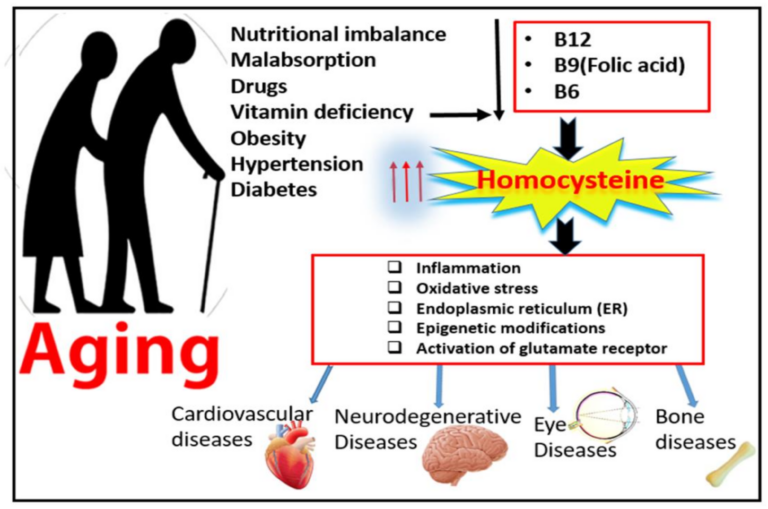
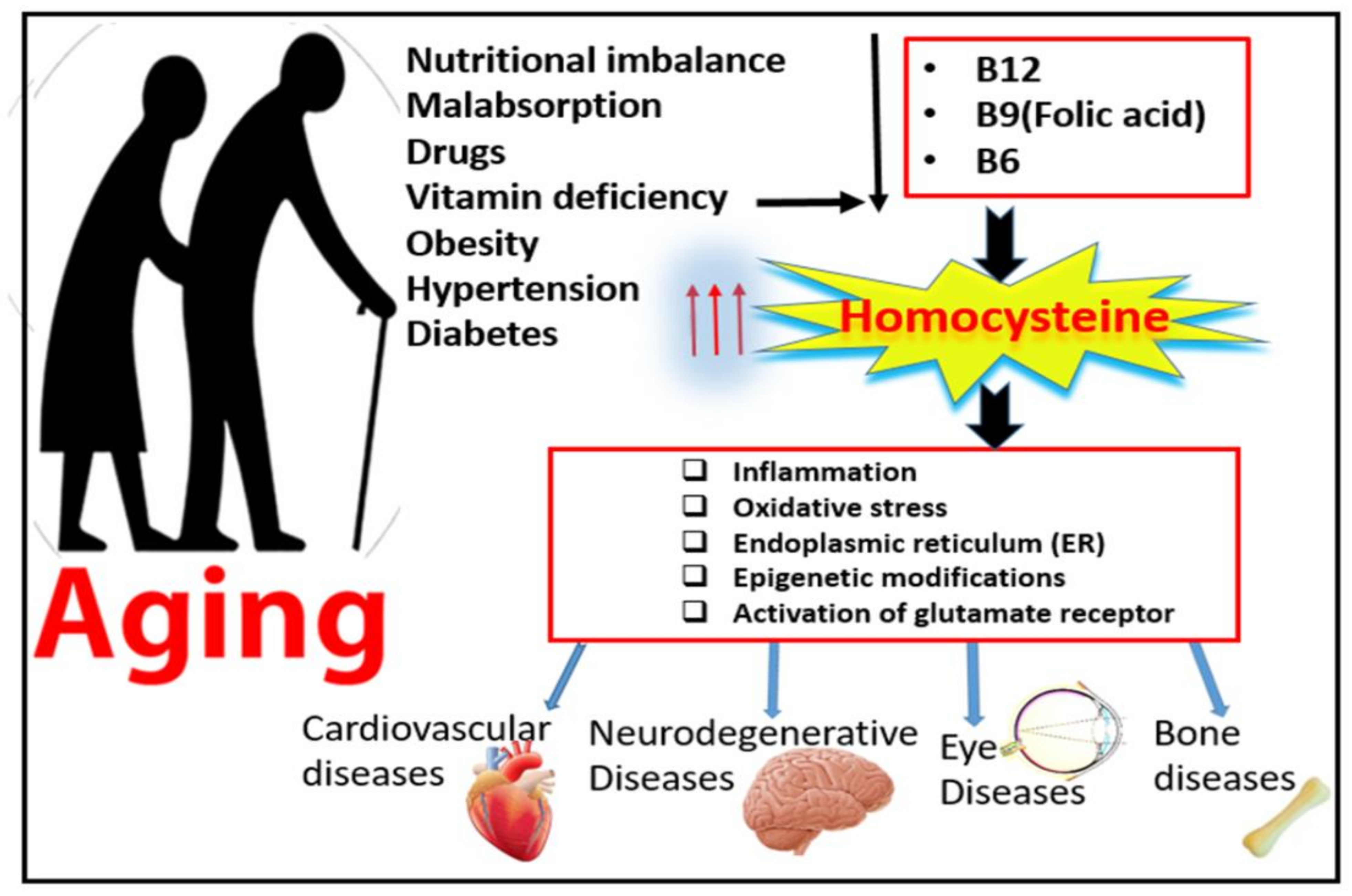
Homocysteine is an amino acid that is produced in the body as a byproduct of methionine metabolism. Elevated homocysteine, also referred to as homocysteinemia, has been linked to an increased risk of cardiovascular disease through several mechanisms:
- Endothelial dysfunction: High homocysteine levels can impair the function of the endothelium, the inner lining of blood vessels. This dysfunction can lead to reduced production of nitric oxide, a molecule that promotes blood vessel dilation and protects against atherosclerosis.
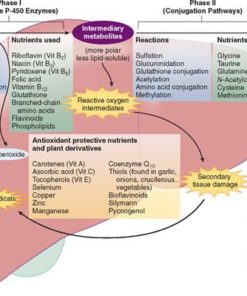
- Oxidative stress: Homocysteine can induce oxidative stress, which can damage blood vessels and contribute to atherosclerosis. Oxidative stress is an imbalance between reactive oxygen species (free radicals) and the body's ability to neutralize them, leading to cellular damage.
- Promotion of blood clotting: Elevated homocysteine levels can increase the propensity for blood clotting by promoting the aggregation of platelets and the activation of clotting factors. This increases the risk of thrombosis and related cardiovascular events, such as heart attacks and strokes.
- Increased inflammation: Homocysteine has been shown to stimulate the production of inflammatory molecules, such as cytokines, which can contribute to atherosclerosis and other cardiovascular problems.
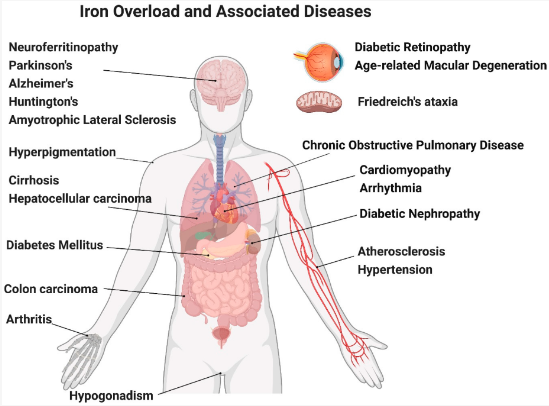
Further emphasizing the importance of addressing elevated homocysteine levels, below is a broader explanation of homocysteine's role in various processes beyond cardiovascular diseases.
- Inflammation: Elevated homocysteine levels can stimulate the production of inflammatory molecules, such as cytokines, chemokines, and adhesion molecules. These molecules can contribute to a pro-inflammatory environment, which can damage blood vessels and other tissues, leading to chronic diseases like atherosclerosis and neurodegenerative disorders.
- Oxidative stress: Homocysteine can induce oxidative stress by promoting the production of reactive oxygen species (ROS) and impairing the function of endogenous antioxidant systems. Oxidative stress can cause damage to cellular components, such as proteins, lipids, and DNA, ultimately leading to cellular dysfunction and tissue damage in various end organs, including the heart, brain, and kidneys.
- Endoplasmic reticulum stress: The endoplasmic reticulum (ER) is an organelle responsible for protein synthesis, folding, and trafficking. Elevated homocysteine levels can disrupt ER function, causing an accumulation of misfolded proteins, a condition known as ER stress. ER stress can initiate a series of cellular responses, collectively called the unfolded protein response (UPR), which can lead to cell death if unresolved. This process may contribute to the development of various diseases, including neurodegenerative disorders and cardiovascular diseases.
- Epigenetic modifications: Homocysteine can interfere with DNA methylation, a key epigenetic mechanism that regulates gene expression. Altered DNA methylation patterns due to elevated homocysteine can lead to changes in gene expression, which may contribute to the development of various diseases, including cancer and cardiovascular diseases.
- Activation of glutamate receptors: Homocysteine can act as an agonist for glutamate receptors, such as the N-methyl-D-aspartate (NMDA) receptor. Overactivation of glutamate receptors can lead to excitotoxicity, a process that results in neuronal damage and cell death. This mechanism has been implicated in the pathogenesis of various neurodegenerative diseases, such as Alzheimer's disease and Parkinson's disease.
C. Cholesterol, Inflammation, and Cardiovascular Risk
Cholesterol is an essential molecule for the body, serving as an antioxidant and the precursor for steroid hormones. Historically, cholesterol has been viewed as the primary cause of cardiovascular disease, leading to dietary recommendations that restrict cholesterol intake. However, recent research has revealed that cholesterol production is often a response to inflammation and oxidative stress.
- The misconception about cholesterol: Rather than being the direct cause of cardiovascular disease, cholesterol production is often the body's attempt to neutralize harmful oxidants. Elevated LDL cholesterol levels are frequently observed in individuals with high consumption of sweets, inflammatory foods, and other sources of oxidative stress.
- Oxidative stress and cholesterol production: Reactive oxygen species, such as those produced by the consumption of refined carbohydrates and sugars, can contribute to inflammation and oxidative stress. This, in turn, can stimulate the production of cholesterol, particularly the "good" HDL cholesterol, to counteract these harmful effects.
- Identifying the true culprits: Rather than focusing solely on cholesterol levels, a more effective approach to managing cardiovascular risk involves identifying and addressing the underlying causes of inflammation and oxidative stress. This includes reducing the consumption of sweets, inflammatory foods, and other sources of oxidants.
II. Identify and Reduce Cardiovascular Risk Factors
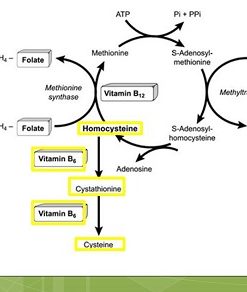
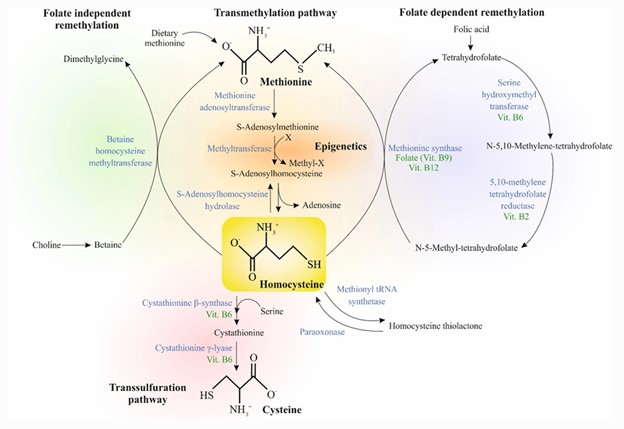
A. Disruptions in Methylation and Transsulfuration Pathways
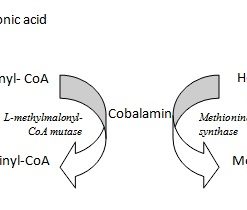
Elevated homocysteine levels can result from impairments in the methylation and transsulfuration pathways, which are responsible for converting homocysteine into methionine and cysteine, respectively. Several factors can lead to impairments in these pathways:
- Nutrient deficiencies: Deficiencies in vitamin B6, B12, or folate can impair the conversion of homocysteine to methionine or cysteine, leading to increased homocysteine levels.
- Genetic mutations: Mutations in genes involved in the methylation and transsulfuration pathways, such as MTHFR, MTR, MTRR, and CBS, can lead to elevated homocysteine levels by impairing the function of enzymes in these pathways.
- Heavy metal exposure: Exposure to heavy metals, such as lead, mercury, or cadmium, can impair enzymes involved in methylation and transsulfuration pathways, such as methionine synthase (affected by mercury) and cystathionine beta-synthase (affected by lead and cadmium).
B. Tests for Determining Homocysteine Levels and Root Causes
Several tests can help identify the source of elevated homocysteine levels:
- Homocysteine test: This plasma-based test measures the total amount of homocysteine in your blood. Elevated homocysteine levels can indicate a potential problem with methylation or transsulfuration pathways.
- Vitamin B6, B12, and folate tests: These tests measure the levels of these essential vitamins in the serum. Deficiencies can impair the conversion of homocysteine to methionine or cysteine, leading to increased homocysteine levels.
- Methylmalonic acid (MMA) test: Elevated serum or urine MMA levels can indicate a functional vitamin B12 deficiency, even when serum B12 levels are normal. This test is helpful because MMA levels are specifically elevated in the case of B12 deficiency, and not in folate deficiency.
- Genetic testing: A genetic test can identify mutations in genes involved in the methylation and transsulfuration pathways, such as MTHFR, MTR, MTRR, and CBS. Certain genetic mutations can lead to elevated homocysteine levels by impairing the function of enzymes in these pathways.
- Heavy metal testing: Tests for heavy metals, such as lead, mercury, or cadmium, can help determine if exposure to these toxins is contributing to elevated homocysteine levels. These metals can impair enzymes involved in methylation and transsulfuration pathways.
- Complete blood count (CBC): A CBC can be helpful in identifying elevated homocysteine levels by revealing macrocytosis, which is characterized by larger-than-normal red blood cells. Macrocytosis can indicate a chronic vitamin B12 or folate deficiency, as both of these vitamins are essential for normal red blood cell production and DNA synthesis.
III. Improve Heart Health with Diet, Lifestyle, and Supplements
A. Homocysteine Diet Tips for a Healthy Heart
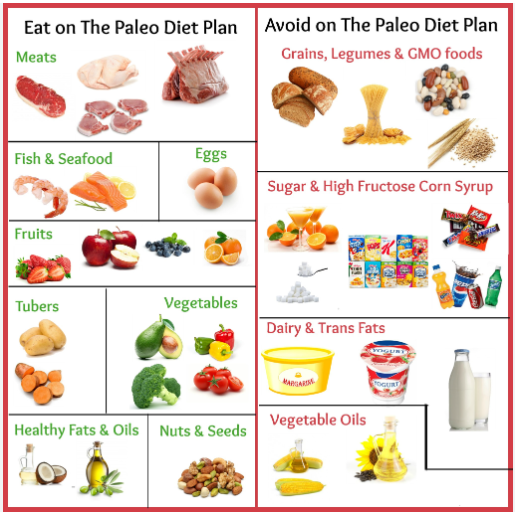
- Adopt a nutrient-dense, anti-inflammatory diet: Focus on consuming a variety of whole, unprocessed foods rich in essential nutrients, including fruits, vegetables, lean protein sources, healthy fats, and complex carbohydrates.
- Avoid refined carbohydrates and sugars: High-carb and sugar-rich foods can contribute to inflammation and oxidative stress, leading to elevated homocysteine levels.
- Include healthy fats: Consume healthy fats from sources like avocado, olive oil, nuts, and seeds, which can support the production of necessary cholesterol and help with absorption of fat-soluble vitamins.
- Exercise regularly: Engage in regular physical activity, which can help improve cardiovascularhealth, reduce inflammation, and support overall well-being.
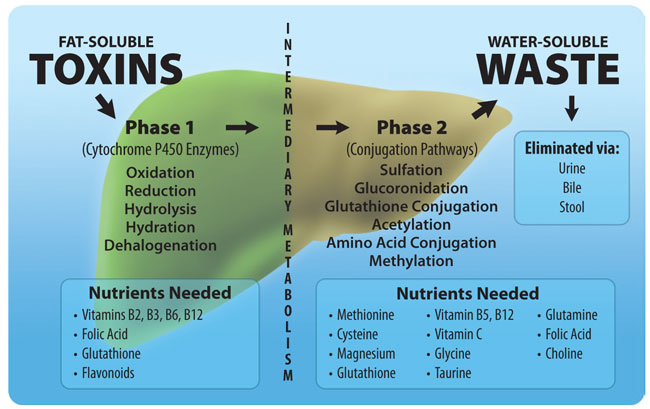
- Practice intermittent fasting: Intermittent fasting may help regulate blood sugar levels, reduce inflammation, and support detoxification pathways.
- Incorporate stress reduction techniques: Stress management is crucial for overall health and can help reduce inflammation and oxidative stress. Consider incorporating practices such as meditation, yoga, or deep breathing exercises into your daily routine.
- Utilize sauna and oxygenation therapies: Regular sauna use can support detoxification pathways and improve cardiovascular health, while oxygenation therapies can help improve circulation and reduce inflammation.
B. Natural Homocysteine Remedies: Supplements for Optimizing Metabolism and Detoxification
- N-acetylcysteine (NAC): NAC is a powerful antioxidant and a precursor to glutathione, the body's primary detoxification agent. Supplementing with NAC can help support the body's natural detoxification processes, lower oxidative stress, and improve glutathione levels, which may in turn help reduce homocysteine levels.
- B vitamins: Supplementing with vitamin B6, B12, and folate can help support proper homocysteine metabolism and address deficiencies that may contribute to elevated levels.
- TMG (trimethylglycine): TMG can help lower homocysteine levels by donating a methyl group to homocysteine, converting it back into methionine.
- Glycine and L-serine: These amino acids can help support the transsulfuration pathway, which is essential for converting homocysteine into cysteine and reducing homocysteine levels.
- Antioxidant support: Antioxidant supplementation, such as with vitamins C and E, selenium, and N-acetylcysteine, can help combat oxidative stress and support the body's natural detoxification processes, potentially lowering harmful heavy metal levels.
- CoQ10: If you are taking statin medications, consider supplementing with CoQ10, as statins can deplete this essential nutrient, which is crucial for cardiovascular health and energy production.
In Conclusion
In conclusion, understanding the role of homocysteine in cardiovascular health is crucial for maintaining a healthy heart and reducing the risk of cardiovascular diseases. By identifying the sources of elevated homocysteine levels and addressing them through targeted dietary, lifestyle, and supplementation strategies, individuals can effectively manage their homocysteine levels and promote overall heart health. By staying informed and making informed choices, we can work towards a healthier future and reduce the burden of cardiovascular diseases in our lives.
Articles Related to Toxicity and Toxicity Therapy
Useful Labs When Evaluating Homocysteinemia
All Cognoscopy Labs
All Cognoscopy Labs
Walsh Approach Test Panels
Walsh Approach Test Panels
Other Single Item Tests