SECOND OPINION SERIES
High Copper Symptoms and the Biochemical Cause
Copper plays essential roles in neurotransmitters, hormones, and antioxidant systems, but when levels become imbalanced—or when too much copper circulates unbound—the nervous system becomes overstimulated. Many patients struggling with unexplained anxiety, irritability, sensory overload, or emotional volatility are actually experiencing high copper symptoms, not a primary psychological disorder.

This Second Opinion Series post explains what high copper symptoms feel like, how copper dumping symptoms appear during treatment or hormonal shifts, why many people experience high copper anxiety that does not respond well to typical psychiatric medications, and which laboratory markers matter most when testing for high copper.
If these patterns sound familiar, there is a clear, evidence-based way to evaluate and improve copper regulation—especially for patients with stress reactivity, hormonal changes, or zinc deficiency.
High Copper Symptoms
When copper rises beyond what the body can bind with ceruloplasmin, the nervous system becomes overly reactive. This creates a distinct picture of high copper symptoms—a combination of emotional intensity, sensory overstimulation, physical tension, and fluctuating anxiety that often worsens with stress, hormones, or inadequate dietary zinc.
High copper amplifies norepinephrine activity, destabilizes dopamine, increases glutamate signaling, and reduces calming GABA tone. The result is a “wired but tired” physiology where the body feels overstimulated even during routine daily tasks.
Common high copper symptoms
-
anxiety that feels amplified or out of proportion
-
irritability, emotional sensitivity, or sudden overwhelm
-
difficulty winding down, insomnia, or restless sleep
-
racing thoughts, internal pressure, or cognitive overload
-
head pressure, nausea, dizziness, or heat intolerance
-
tension in the jaw, shoulders, or chest
-
PMS worsening, postpartum shifts, or mid-cycle emotional crashes
These high copper symptoms often fluctuate rather than remain constant. Many patients describe periods where everything feels louder, more intense, or harder to regulate—followed by temporary relief before symptoms build again.
Copper Dumping Symptoms
Copper dumping symptoms occur when stored copper begins moving into circulation faster than the body can bind and excrete it. This typically happens during zinc therapy, postpartum recovery, discontinuation of a copper IUD or estrogen-containing birth control, rapid weight loss, detoxification phases, or periods of high physiological stress.
As copper mobilizes, norepinephrine surges temporarily, and glutamate/GABA balance shifts. This causes short-lived but intense symptoms that often alarm patients unless they understand the mechanism.
Common copper dumping symptoms
-
abrupt spikes of irritability, agitation, or emotional intensity
-
nausea, metallic taste, or sudden head pressure
-
flushing, heat waves, or sweating
-
temporary insomnia or vivid, restless dreams
-
fatigue following an episode due to neurotransmitter depletion
-
short-term worsening of high copper symptoms
Copper dumping symptoms do not indicate treatment failure—they are evidence that copper is shifting from tissues toward elimination. The key is pacing, zinc stabilization, and supporting ceruloplasmin production so dumping remains manageable.
High Copper Anxiety
Copper-driven anxiety is distinct from generalized anxiety disorder. Excess copper exaggerates norepinephrine output, destabilizes dopamine, increases excitatory glutamate activity, and reduces inhibitory GABA tone. The result is high copper anxiety—a pattern marked by agitation, sensory overload, and emotional intensity rather than quiet worry or rumination.
Patients often report that this form of anxiety feels physical, electrical, or internally pressured. Many also respond poorly to benzodiazepines or SSRIs because these medications do not correct the underlying neurotransmitter imbalance.
Why high copper anxiety happens
-
Norepinephrine dominance → hyper-alertness, startle reactions
-
Dopamine instability → poor stress tolerance, racing thoughts
-
Glutamate excess → sensory overload, cognitive rigidity
-
Reduced GABA tone → difficulty relaxing, internal tension
-
Oxidative stress → irritability and inflammation-driven reactivity
These mechanisms explain why high copper anxiety often appears in puberty, pregnancy, postpartum, perimenopause, after stressful life events, or when dietary zinc is very low.
Testing for High Copper
Accurate evaluation requires more than looking at total copper levels. Many patients with severe symptoms have “normal” total copper but elevated unbound copper—the biologically reactive form that influences neurotransmitters.
Anyone experiencing high copper symptoms, copper dumping symptoms, or high copper anxiety should consider testing for high copper using the combination below.
Key labs for testing for high copper
-
serum/plasma copper
-
ceruloplasmin (required to calculate free copper)
-
free copper (calculated value showing reactive copper load)
-
plasma zinc & zinc:copper ratio
-
whole blood histamine (optional but highly informative for stress reactivity)
-
SAM/SAH methylation panel if symptoms are severe, long-standing, or resistant
Testing clarifies not only whether copper is elevated, but why—low zinc, low ceruloplasmin, high estrogen exposure, inflammation, stress, cookware/water exposure, or nutritional imbalance.
Mechanisms Behind High Copper Symptoms
Copper biology is far more complex than “too much copper causes anxiety.” Modern neurochemistry—and Walsh’s updated interpretations—show that copper influences neurotransmission, oxidative stress, hormone handling, amino acid transport, and inflammatory pathways. The following expands each mechanism with appropriate scientific depth while remaining clinically accessible.
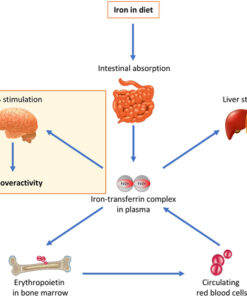
1. Copper, Catecholamines & DBH Regulation
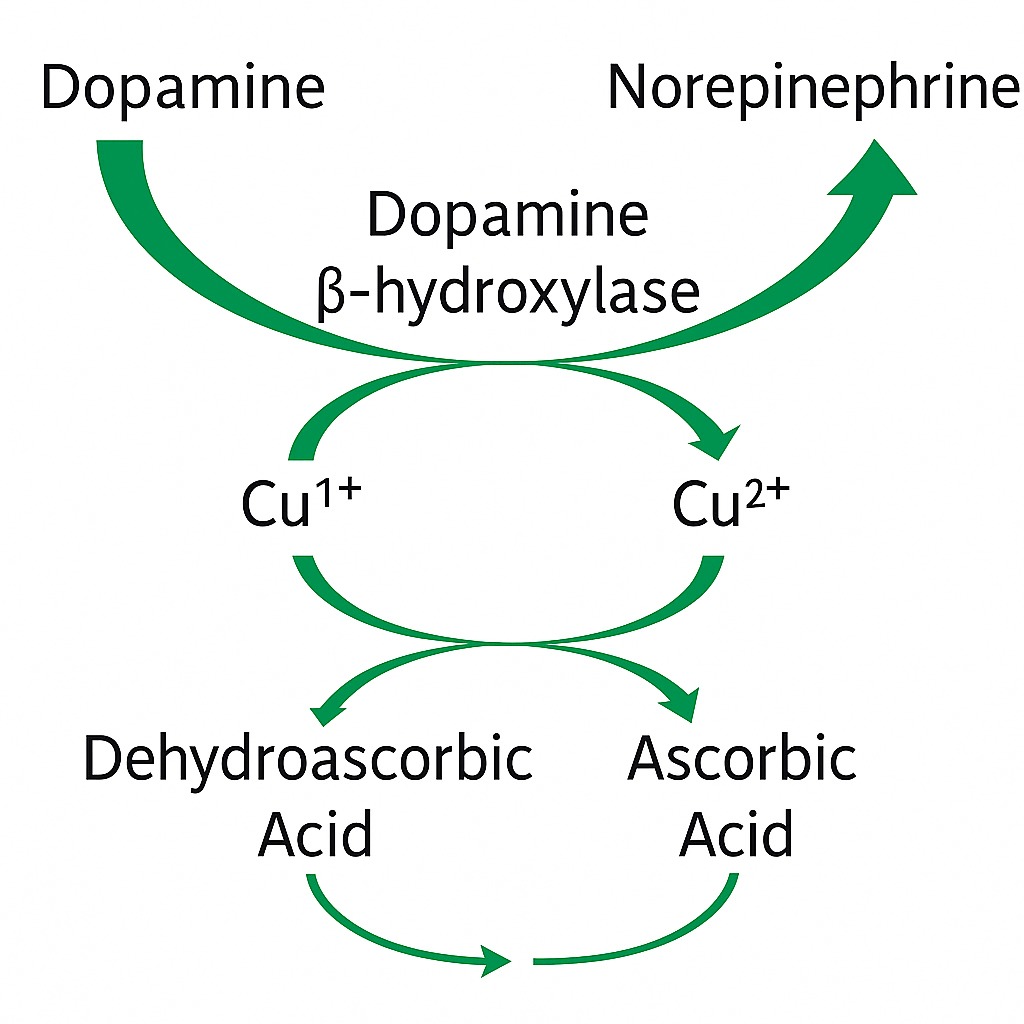
For decades, clinicians believed high copper accelerated dopamine-β-hydroxylase (DBH), increasing conversion of dopamine → norepinephrine. Modern enzymology shows this is incorrect: DBH saturates at relatively low copper concentrations. Excess copper does not speed the enzyme; it disrupts neurotransmitter handling upstream and downstream.
How high copper actually increases norepinephrine activity
-
Vesicular dysregulation: Copper alters the packaging and release of DBH-containing vesicles, causing inconsistent norepinephrine release that feels like surges of agitation or hyper-alertness.
-
Dopamine instability: Oxidative stress from free copper degrades dopamine before it can be used, lowering resilience and shifting the overall catecholamine balance toward norepinephrine dominance.
-
Synaptic misregulation: Copper disrupts feedback loops controlling norepinephrine reuptake and auto-inhibition, creating persistent sympathetic “pressure.”
-
Reduced antioxidant buffering: Low glutathione (common when copper is high and zinc is low) reduces the brain’s ability to stabilize dopamine and protect synapses under stress.
Clinical significance
Patients with high copper often present with:
-
racing thoughts
-
irritability
-
internal agitation
-
panic sensations without clear trigger
-
intolerance to stimulants or stressful environments
These symptoms correlate strongly with high copper anxiety, not primary psychiatric disease.
2. Copper, Glutamate & NMDA Receptor Hyperactivity
Glutamate is the brain’s primary excitatory neurotransmitter. In a healthy system, glutamate is tightly regulated by transporters (EAAT1–5), astrocytes, and enzymatic recycling. When copper is elevated, these systems weaken, and excitotoxic pressure builds.
How copper disrupts glutamate regulation
-
Reduced EAAT transporter efficiency: Free copper interferes with astrocytic glutamate uptake, allowing glutamate to accumulate between neurons.
-
NMDA receptor sensitization: Copper indirectly modifies NMDA receptor kinetics, increasing receptor responsiveness even without higher glutamate release.
-
Impaired inhibitory balance: High copper weakens GABA-A receptor function—especially in zinc-deficient states—removing the braking system that normally counterbalances NMDA activity.
-
Neuroinflammation amplification: Copper-induced ROS (reactive oxygen species) activate microglia, which further increase glutamate release and NMDA tone.
Clinical significance
This mechanism explains:
-
sensory overload
-
cognitive rigidity
-
overstimulation in crowds or noise
-
insomnia from inability to “shut off” neural activity
-
agitation that worsens with stress
This is the neurological backbone of high copper symptoms.
3. Free Copper, Ceruloplasmin & Hormonal/Inflammatory States
Total copper alone is misleading; the biologically relevant form is free (unbound) copper, which increases when ceruloplasmin is low. Ceruloplasmin synthesis depends on protein status, methylation support, liver health, and inflammatory signaling.
Why free copper rises
-
Low ceruloplasmin: Estrogen exposure, stress hormones, inflammation, and nutritional deficiencies reduce CP synthesis.
-
Excess estrogen: Birth control, hormone replacement therapy, pregnancy, and postpartum shifts raise copper absorption and retention.
-
Liver load: Mold exposure, chronic infections, and fatty liver lower ceruloplasmin, increasing unbound copper.
-
Protein deficiency: Inadequate dietary protein impairs ceruloplasmin production, leaving copper biologically reactive.
Clinical significance
Elevated free copper is associated with:
-
PMS and PMDD
-
postpartum anxiety
-
sudden emotional volatility
-
hypersensitivity to stress
-
insomnia and night-time agitation
-
worsening of OCD-like rigidity or intrusive thoughts
These are key elements of high copper anxiety and cyclical copper sensitivity.
4. Oxidative Stress, Glutathione & Antioxidant Collapse
Copper participates in redox cycling. When copper exceeds safe binding capacity, it drives the Fenton reaction, producing hydroxyl radicals that rapidly damage lipids, proteins, and neurotransmitters.
How oxidative stress contributes to symptoms
-
Dopamine degradation: ROS degrade dopamine in synapses, impairing reward pathways and stress recovery.
-
Reduced glutathione: Copper overload depletes glutathione, the brain’s primary antioxidant, increasing vulnerability to inflammation and stress.
-
Mitochondrial strain: Copper-induced oxidative stress impairs mitochondrial ATP output, contributing to fatigue, irritability, and cognitive slowing.
-
Inflammation-amplified reactivity: High oxidative stress lowers the threshold for emotional triggers, intensifying high copper symptoms.
Clinical significance
Patients often describe:
-
“wired and tired” physiology
-
emotional fatigue
-
brain fog or overwhelmed processing
-
difficulty regulating reactions
These oxidative pathways also heighten copper dumping symptoms when mobilization increases ROS temporarily.
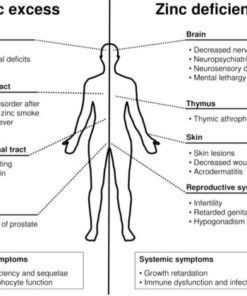
5. Zinc Deficiency, Metallothionein & Copper Retention
Zinc is the primary regulator of copper homeostasis. Metallothionein, a zinc-dependent protein, binds and eliminates copper. When zinc is low, copper accumulates—even if intake is normal.
How zinc deficiency worsens copper imbalance
-
Reduced metallothionein: Copper cannot be properly bound or excreted, raising free copper.
-
GABA implications: Zinc modulates GABA-A receptors; deficiency decreases inhibitory tone, worsening anxiety.
-
Glutamate implications: Zinc naturally dampens NMDA receptors; low zinc permits excess excitatory signaling.
-
Immune & gut factors: Low zinc increases permeability and inflammation, further affecting ceruloplasmin and neurotransmission.
Clinical significance
Zinc deficiency is nearly universal in those with:
-
pyroluria
-
chronic stress
-
vegan/vegetarian diets
-
malabsorption
-
prolonged inflammation
Zinc restoration is often the single most impactful component of recovery.
6. Dietary & Environmental Copper Exposure
Exposure alone rarely causes high copper symptoms, but exposure + weak regulation is the formula for trouble.
Major environmental contributors
-
well water with high copper content
-
acidic water through copper pipes leaching metals
-
copper cookware, especially with acidic foods
-
high copper foods (shellfish, organ meats, chocolate, nuts, seeds) combined with low zinc diets
-
fertilizers, fungicides, or older plumbing contributing to chronic intake
Clinical significance
These exposures matter most when ceruloplasmin is low or metallothionein is impaired. Many cases of high copper anxiety are due not to excess intake but to poor copper handling capacity.
7. Hormonal States That Exaggerate Copper Effects
Copper rises significantly in the presence of estrogen. This is physiologic—but problematic when regulation is already weak.
High-risk hormonal states
-
starting or stopping estrogen-containing birth control
-
copper IUD use
-
pregnancy (especially 3rd trimester)
-
postpartum period (sharp drop in ceruloplasmin)
-
perimenopause or high-estrogen cycles
Clinical significance
These shifts commonly precipitate:
-
postpartum anxiety
-
cyclical irritability or emotional crashes
-
worsening sensory sensitivity
-
panic episodes not present before hormonal change
These features represent classic high copper symptoms, often misdiagnosed as PMDD, GAD, or postpartum depression without copper testing.
8. Why Copper Dumping Occurs During Treatment
Zinc repletes metallothionein, which begins mobilizing stored copper from tissues into the bloodstream. This rapid shift causes temporary instability.
Mechanisms behind copper dumping symptoms
-
increased free copper during mobilization
-
temporary rise in norepinephrine activity
-
glutamate/GABA imbalance during copper redistribution
-
oxidative load from copper movement
-
neuroinflammatory reactivity
Clinical significance
Copper dumping symptoms show that the copper regulation system is reawakening, not failing.
RESEARCH: For a medically reviewed overview of how excess copper affects the nervous system, oxidative stress, and clinical symptoms, see the NIH/StatPearls article Copper Toxicity, which provides a clear summary of copper metabolism and its impact on health.