Managing Histamine Intolerance with Methylation & Nutrient Therapy
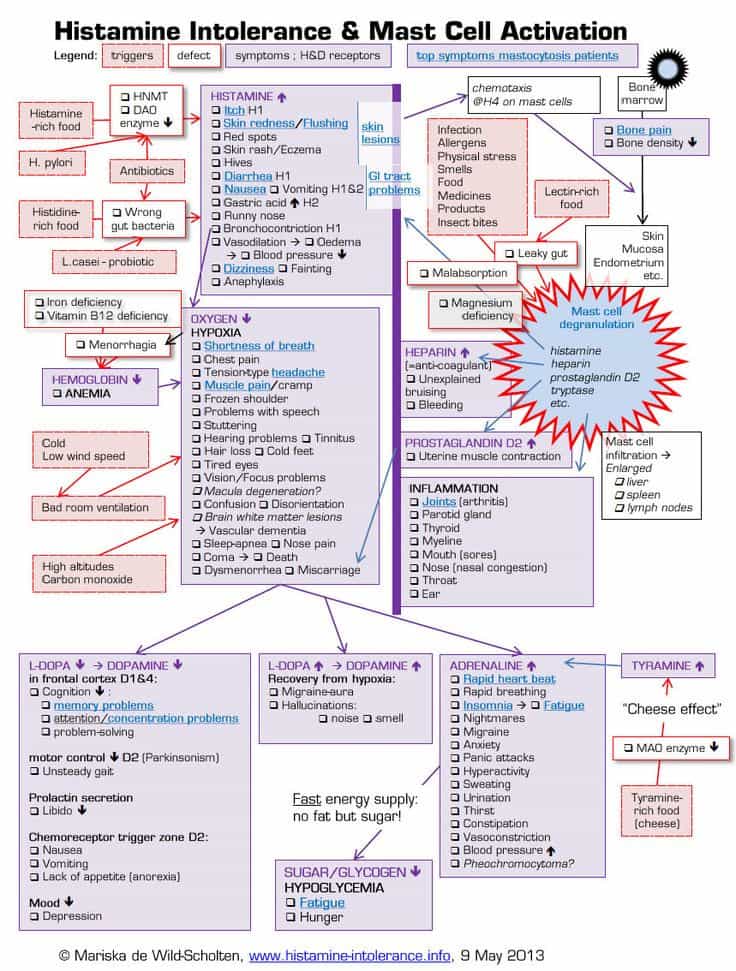
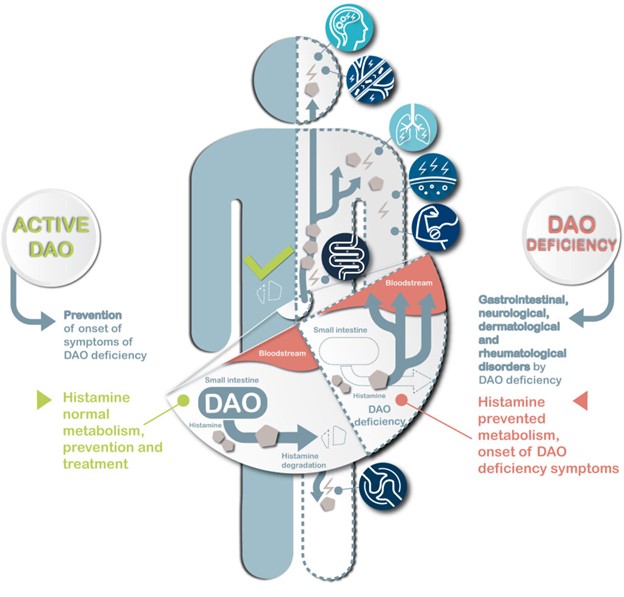
Histamine intolerance is a condition in which the body accumulates an excessive amount of histamine. This compound plays a vital role in our immune response and is responsible for triggering inflammation when the body is under attack. However, in some people, histamine can accumulate due to a variety of reasons, such as an underactive enzyme that breaks down histamine or overproduction of histamine in the body. The accumulation of histamine can result in various symptoms ranging from mild to severe, including migraines, gastrointestinal problems, and skin rashes. In this article, we will discuss the importance of methylation in managing histamine levels and explore the various treatment options available, including diet modifications, supplementation, and probiotics.
Understanding Histamine Intolerance
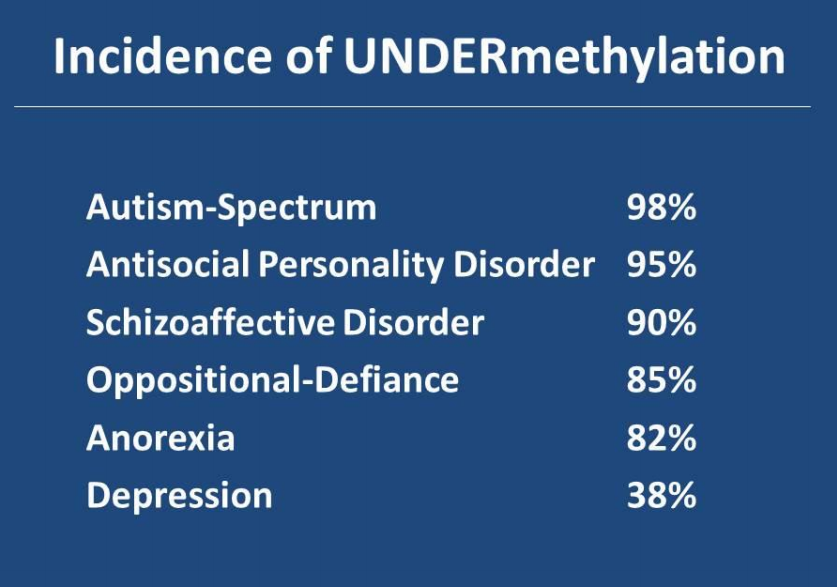
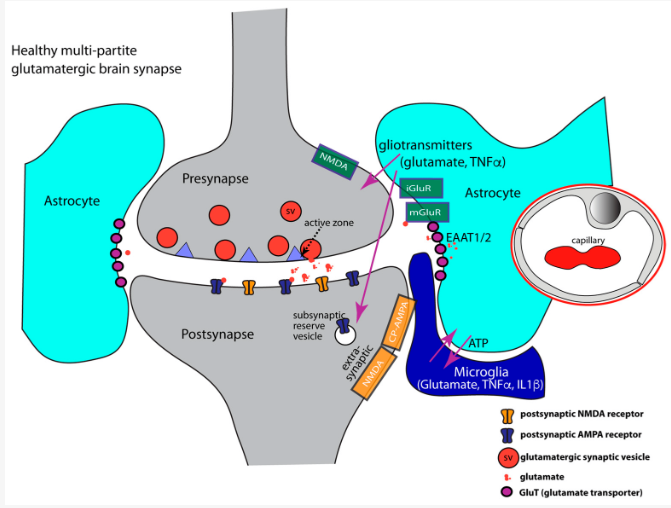
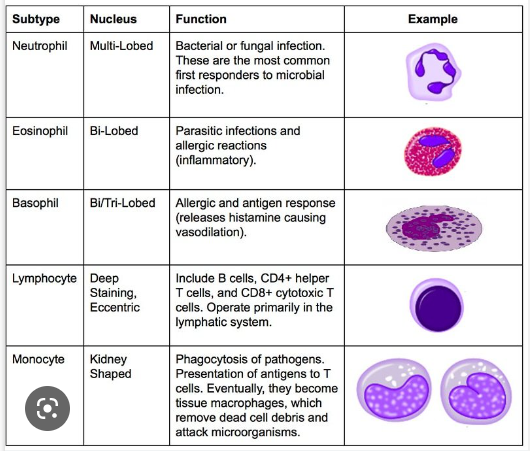
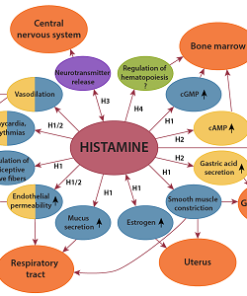
Histamine intolerance is commonly associated with symptoms such as respiratory issues, gastrointestinal problems, and skin rashes due to the build-up of histamine in the bloodstream. However, it is important to note that histamine intolerance can also affect neurological functions, as histamine is involved in neurotransmitter regulation. In particular, histamine is a key modulator of serotonin and dopamine activity, both of which play important roles in mood regulation through the activity of reuptake enzymes DERT and SERT. Therefore, measuring whole blood histamine levels can provide an estimation of the activity of these important neurotransmitters and help identify the potential impact of histamine intolerance on neurological symptoms and mood disorders.
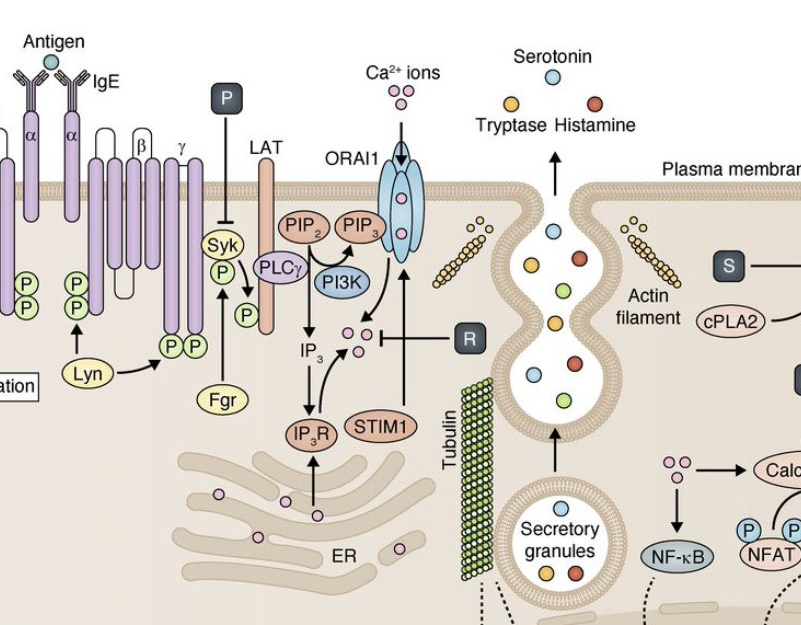
It is worth noting that in addition to histamine intolerance, mast cell activation disorder (MCAD) is another condition that can lead to an excess release of histamine and other mediators from mast cells. MCAD is a complex and often underdiagnosed condition that can cause a wide range of symptoms, including gastrointestinal disturbances, headaches, fatigue, skin rashes, and neuropsychiatric symptoms such as anxiety and depression. Research suggests that impairments in the methylation cycle may be involved in mast cell dysfunction and the development of MCAD. Therefore, measuring whole blood histamine levels and assessing methylation status may be important considerations for individuals with suspected MCAD.
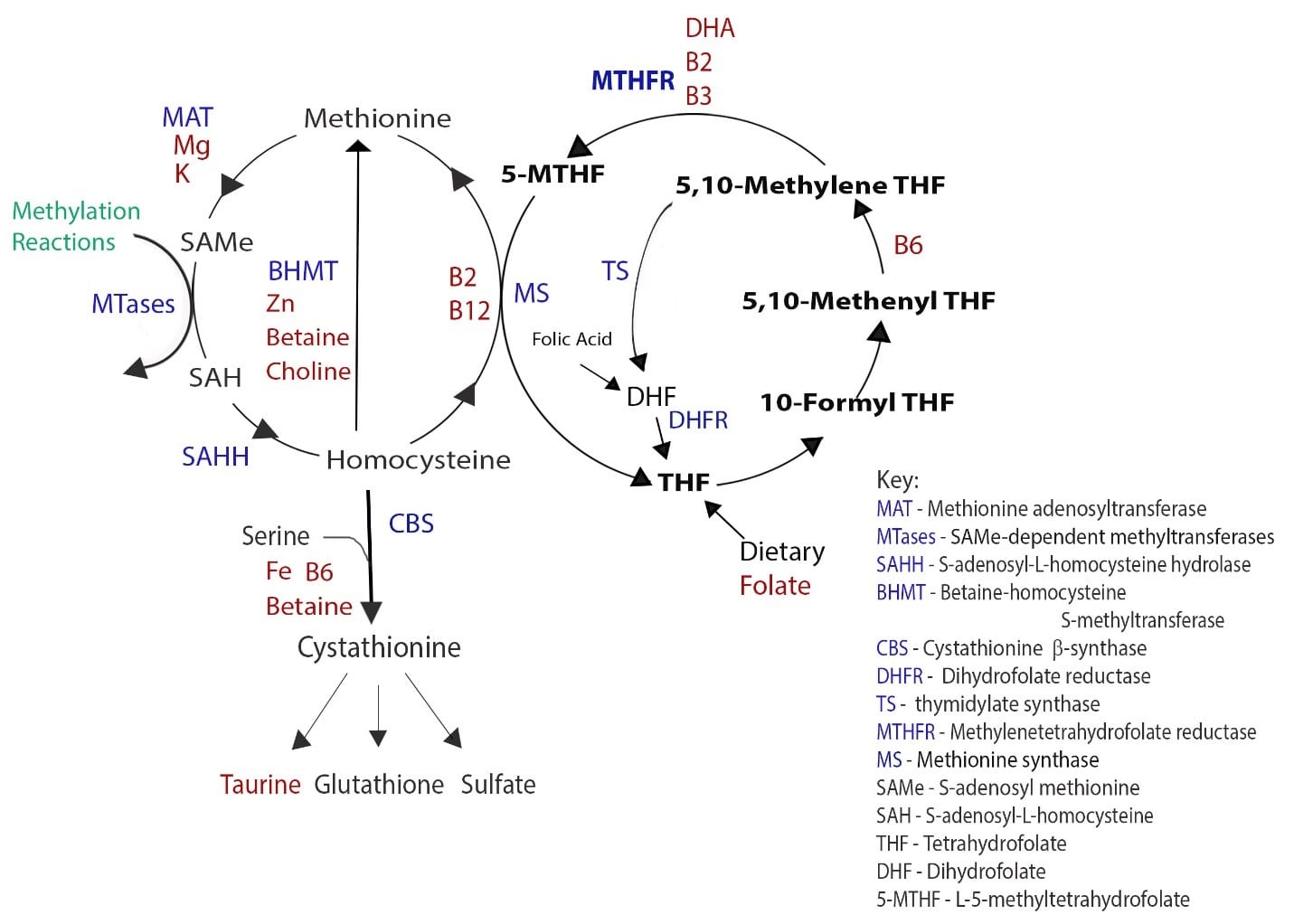
The Role of Methylation in Managing Histamine Levels
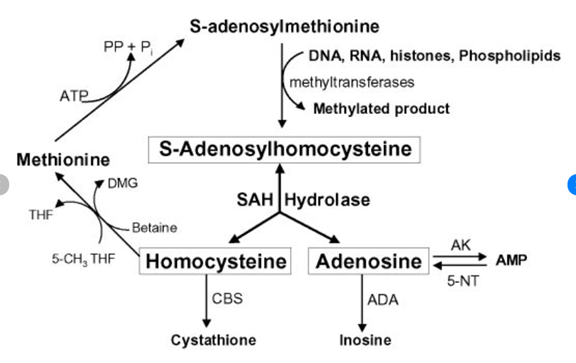
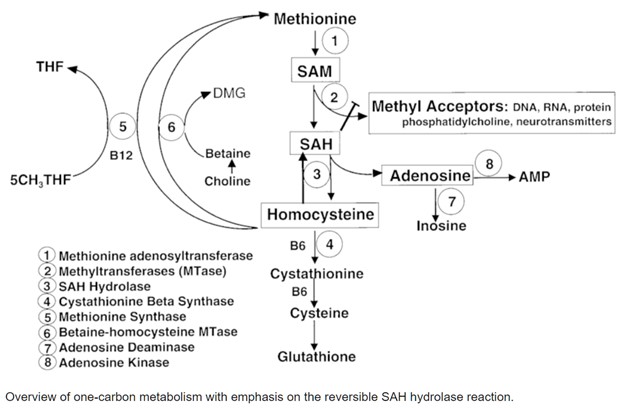
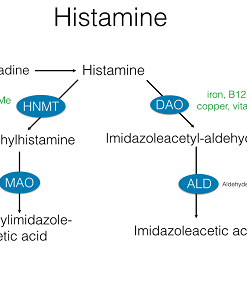
The one-carbon cycle, or methylation cycle, is a complex biochemical process that plays a key role in the regulation of many bodily functions, including the management of histamine levels. The cycle involves the transfer of a methyl group (CH3) from one molecule to another, which is facilitated by enzymes that are dependent on certain vitamins and nutrients, such as folate, vitamin B12, and SAMe. This cycle is responsible for many important processes, including the synthesis of DNA, RNA, and neurotransmitters, as well as the regulation of gene expression. Detecting methylation status can help identify imbalances in this cycle, which can lead to histamine intolerance and other health issues. By supplementing with nutrients that support methylation, such as folate and B12, and by avoiding factors that interfere with the cycle, such as toxins and stress, methylation can be improved, which can help manage histamine levels and reduce symptoms associated with histamine intolerance.
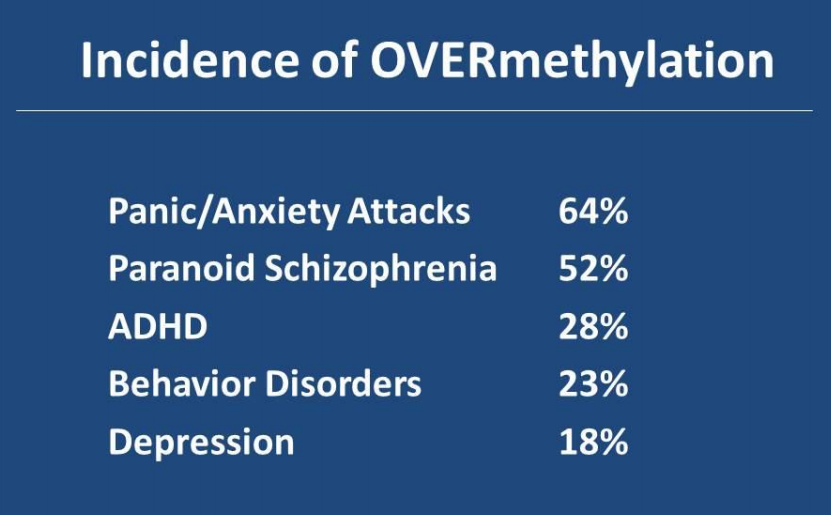
Testing for Undermethylation and Overmethylation
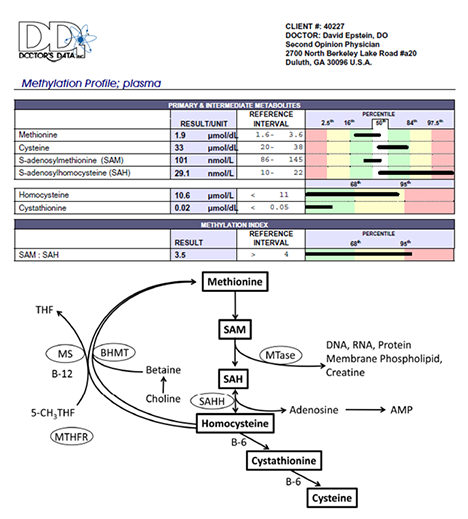
At this Second Opinion Physician website, patients can order the necessary testing to determine their methylation status and evaluate for overmethylation or undermethylation. It is important to note that MTHFR genetic testing is generally not useful in determining methylation status. Instead, the Walsh protocol is used to measure whole blood histamine and plasma methylation levels. This testing is especially important for patients experiencing mood disorders, which can be exacerbated by supplementation to increase or decrease methylation. With the results of these tests, nutrient therapy can be tailored to the patient's specific needs and symptoms, improving methylation and reducing symptoms associated with histamine intolerance.
Histamine Intolerance and Diet
Histamine intolerance is a condition where there is an accumulation of histamine in the body which can cause a range of symptoms such as headaches, itching, hives, and gastrointestinal issues. Foods high in histamine or histamine-releasing foods can trigger these symptoms in people with histamine intolerance. Fermented foods such as sauerkraut, yogurt, and kimchi are typically high in histamine due to the presence of histamine-producing bacteria. Certain types of fish, aged cheese, and processed meats also contain high levels of histamine. It's important to pay attention to food labels and avoid foods that trigger symptoms.
In Conclusion
In conclusion, histamine intolerance is a complex condition that can result in a variety of symptoms, including respiratory issues, gastrointestinal problems, and skin rashes. Testing for histamine levels, as well as methylation status, can be helpful in charting a plan to manage histamine intolerance. Supplementation with nutrients such as DAO, SAMe, methionine, magnesium, biotin, B12, TMG, vitamin B6, NAC, and folic acid can help improve methylation and reduce symptoms associated with histamine intolerance. It's important to work with a healthcare provider who understands the complexities of histamine intolerance and can guide patients in developing a personalized treatment plan. Additionally, paying attention to food labels and avoiding foods that trigger symptoms can also be helpful. Overall, with proper testing and management, individuals with histamine intolerance can experience relief from their symptoms and improved quality of life.
Symptoms of Elevated Whole Blood Histamine
Symptoms of Low Whole Blood Histamine
Second Opinion Histamine and Methylation Tests
Walsh Approach Single Tests
Walsh Approach Test Panels
Methylation Test Panel – Whole Blood Histamine & Homocysteine
Walsh Approach Test Panels




Hi, o have interest of knowing more about the probiotics thay increase and the others crpas that decrease histamine. Do you have the references? Thank you só much!
I have been suffering from high histamine issues…primarily hives and insomnia…ever since taking a round of Cipro. I’m waiting for my Dutch hormone testing but I already know my estrogen is extremely high and I have almost no progesterone. I’m taking Taurine, GABA, vitamin C, B-6, and zinc. I have a hunch I have low cortisol…I have always lived an extremely fast paced, super-stressed lifestyle. While I wait the 2-3 weeks for my Dutch results, will it hurt to take the taurine and GABA to calm my anxiety? I don’t want to lower my cortisol if it’s already too low…I can’t afford for my Histamine levels to get any worse.
Excellent and helpful article…Can you recommend a physician in Naples,FL who could help treat my adult daughter ? We were recently exposed to significant mold ( that she is allergic to) in our house. We are out of the house until this can be remediated next Wed. Any recommendations would be greatly aporeciated.
This is a great article but some of the things mentioned are things found to be high in glyphosate and glufonisate which has been found to raise histamines. They use those herbicides to dry beans and grains. Also people may want to avoid GM products because it has been found the body reacts to the BT Toxin in them the same way they would if you had food poisoning.
This is excellent! Right on the money when it comes to explanation and advice to help. Thank you so much for publishing this.
Great,informative post ,thanks.
What is the best DAO Enzyme Supplement to take?
I find that so many who suffer with histamine problems are also sensitive to salicylates, and it is important to learn about oxalates. The best place to learn about oxalates is “Trying Low Oxalates TLO” facebook group and other groups Susan Owens is the expert. Oxalates cause kidney stones, gout, leaky gut, eye problems, joint pain, lower minerals and sulfur, if this isn’t addressed the other problems persist. Also iodine helps control histamines– and important to note meat must be very fresh (for histamines) so buy fresh and freeze right away. (No leftovers) Iodine info–https://www.youtube.com/watch?v=seymLq1ofXA– also, environmental stress is a trigger to histamine release– heat, cold, mold, … many also fine OMAD (one meal a day helps) and Intermittent fasting– at least 18 hours a day of clean fasting (Plain water only) gives the body a chance to heal — Dr. Jason Fung –“Intermittent fasting … That is the process of autophagy, where sub-cellular organelles are destroyed and new ones are …”
Hi
Thank you for the article. Well done.
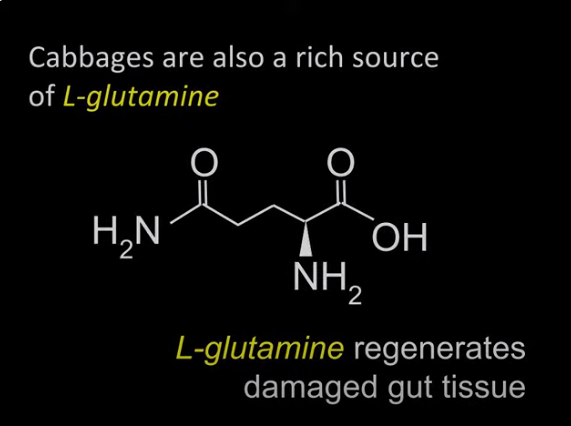
I have a very complex situation. I suffer from gastritis. Had my gallbladder removed do to a pancreatic attack. Everything normalized , but I continue suffering from leaky gut, gastritis, gerd post nasal drip, possible ulcers lots of burning in the gut.
Recently developed a nagging pain that I believe may be an ulcer. I began taking Carnosine Zinc and I feel it helps my stomach, but I notice when I take carnosine the histidine makes my histamine worse. I also am gluten intolerance and recently also developed a geographical tounge which we think was a fungus infection. I was given several doses is Nystatin and Diflucan which only made it worse. I did take antibiotics a while back. I believe the Zinc carnosine can help me, but I need to balance my micro flora and control my histamine level. When I take Zinc Carnosine I get severe pain in my joints and an ache feeling as if I took gluten. My sinus are also very dry and I am always dehydrated regardless if I drink water. My E&T doctor says I have allergies but I have not suffer ed from any rashes or asthma just very dry sinus and post nasal drip. I also suffer from gerd if the acid gets out of control. Based on your article it appears I was taking the wrong probiotics.
I would dearly appreciate any suggestion or recommendation you may have.
Thank you,
Christine
Christine, thanks for your comment. It would be difficult to assess your situation from this information alone, and it would not be appropriate for me to do so in this comment section. Suggest that you have a Comprehensive Digestive Stool Analysis x 3 (I use Doctors Data) completed and start with identifying status of your digestive tract flora, parasites, yeast and food digestion. Nasal drip will disrupt the protective gastric mucosa and lead to leaky gut and a worsening of the sinus drainage. You might ask your doctor about chromalyn sodium, aka Nasalchrome. A low carb, low fruit, paleolithic diet along with a broad spectrum probiotic and other digestive support supplements should also give you some relief.
Thanks for your question, however, it would not be appropriate for me to make medical recommendations via public chat without taking proper history and necessary labs.
Allergy Research has a grass fed beef glandular that is offered at Biotype Nutrients, a website managed by Second Opinion Physician.
Yes, you are correct when it comes to whole foods. It is important to source organic products whenever possible to avoid glyphosates. Supplements however are not commonly available as organic. Fortunately dosages are much smaller than the source agriculture product and extracts do not likely contain glyphosates.
Thank you
Glad you found it helpful.
Thank you Jennifer, these are all excellent points. In regards to metals it is also important to consider copper, as it is a component of DAO. However, too much copper can also cause anxiety and ADHD, particularly if diet is inadequate or the body is low in metallothionines such as ceruloplasmin which bind free copper. Important to test copper levels prior to taking copper supplements. And a good idea to test RBC magnesium prior to taking iodine.
Pingback: Histamine Intolerance
Hi,
I was looking at the information on your website as I am researching to help with issues my 8yo son is suffering from…..chronic infections, chronic fatigue, rashes, chronic abdominal pain and vomiting. After much begging, we did additional blood work.
Histamine Level= 4913 nmol/L
Zinc= 77 ug/dl
Copper= 115 ug/dl
Cortisol (9am)= 5.4 ug/dl
Ferritin= 21 ng/ml
Any recommendations?
Thanks
Amanda
I hope this helps. Feel free to send an email to info@secondopinionphysician.com if you’d like to schedule a free pre-consultation with the doctor.
I have a history of Paroxysmal Atrial Fibrillation. A cardiologist said that he would normally do an ablation because of the number of episodes I had had but considering that I was on a blood thinner and have a high BMI he felt that proper pressure could not be applied at the catheter insertion site and that I could bleed and bruise excessively post ablation. So in spite of an anti arrhythmic I still had episodes. I read as much as I could and found that histamine excess due to a decrease in DAO production in older people can trigger A Fib. I have modified my diet to reduce histamine producing foods and rarely have break through A Fib. My cardiologist is skeptical. Is there a peer reviewed article that mentions excess histamine as an A Fib trigger that I can share with her?
They have several benefits and I would like to try some of them. I didn’t know they have this excellent benefits other than they are nutritious.
Missy if you are injured from Cipro it may be wise to take P5P instead of straight B6, B6 can make any neuropathy much worse. Im not a Dr just a fellow Floxy that learned the hard way lol.
Do you think rosacea can be linked to histamine and Mast Cell Activation Disorder? I’m wondering what test and/or supplement I could take to see if there is a correlation?
I would consider testing for copper overload and maybe a GI evaluatio. Rosacea tends to arise from intestinal inflammation and zinc deficiency. zinc/copper/ceruloplasmin
Where is the published research or Pubmed study or studies that show methionine lowers histamine levels. Thanks in advance.
I cannot provide specific medical recommendations by open forum, however, the histamine we use in determining methylation status is from Whole Blood; this test was for plasma or serum. Judging from these labs there is a sufficient copper imbalance to suggest supplementation will be helpful for various mood disorders (none indicated in your comment). Whether or not the histamine or oxidative stress is contributing to rashes, pain, vomiting etc would have to be determined through more detailed assessment and supplements trial.
You may wish to peruse the studies that indicate SAMe is the rate limiting factor behind 220 of 230 known methyltransferase activities. Histamine methyl transferase is the enzyme that lowers histamine within the red blood cells. By deduction, it is strongly argued that that reduced SAMe (methionine source) or low methylation will result in higher whole blood histamine. Here’s a usedful link: https://www.sciencedirect.com/topics/neuroscience/methyltransferase “3.1 Assay Formats – Methyltransferases utilize SAM as a methyl donor, regardless of their substrates as proteins, nucleic acids, or small-molecule substrates, and with the formation of SAH as a by-product (Carmel, Jacobsen, & Hajjar, 2001).”
The histamine is not a whole blood histamine fraction. Evidently the sample was a plasma or serum specimen. Suggest retesting that for methylation status. We like to see a range of 40-70 for normal, assuming no antihistamines (including histamine lowering anti-depressants) were taken within a month prior to the labs. Higher levels of histamine suggest undermethylation, lower suggest overmethylation. Remember, it is not advisable to take folates for undermethylation or for high histamine when addressing mood disorders, because they increase the reuptake of serotonin and dopamine, lowering the action of these neurotransmitters. Zinc and copper levels should be flipped Zinc/Copper ratio of 1.25 is ideal. In this case the Copper/Zinc ratio is too high. Use caution when treating low zinc/high copper. Testing ceruloplasmin when testing copper is needed to determine free copper.
It certainly could be related. I also see a lot of folks who have zinc deficiency with rosacea. The digestive tract is a good place to start.
suggest searching the NIH website: pubmed.gov
So you mention that in under methylation one should not take folates in mood disorder because it lowers serotonin. I’m confused by this, if I was under myth elating wouldn’t I need folate? What about b vitamins that are already methylated?
‘Methylated’ B Vitamins are not a factor in contribution of total methyl compounds. They are advisable when genetic test suggests need for methylated, assuming one does not have low serotonin ACTIVITY, based on Walsh test measure of whole blood histamine. This is key, methylation may increase the production of serotonin, but folates lower the activity. The same goes for persons with chronic low levels of zinc or vitamin B6, common with pyroluria. These are considered to be low serotonin ‘level’ conditions. If low levels or low activity exists then folates, like niacin and DMAE are discouraged when patients are suffering from low serotonin or low dopamine mood and/or behavior disorders. If there is reason to believe the need to supplement with folates (pregnancy planning, macrocytosis, etc) outweighs the risk of lowering serotonin activity then this information must be reconsidered, case by case.
Thank you for this information, it has helped me immensely.
My whole blood histamine is elevated 1,722 nmol/L/191.4 ng/mL (serum was recently 0.29 ng/mL). I’ve been working on it over a year and have gotten it down from 2,541 nmol/L.
Copper is 1.2 ug/mL (120 ug/dL),
Ceruloplasmin 24 mg/dL,
rbc zinc 10.8 mg/L
Eosinophil % 7 (was 17 – shot up suddenly 11/2018)
This started after I had surgery and the doc recommended a vegan diet and prescribed Metformin for my A1C of 6%. I followed the diet but became sick from the Metformin and then malnourished from the diet and the messed up gut from the Metformin. She also advised me to take probiotics. Unfortunately, I believe many were high histamine probiotics. I have since stopped listening to her (and ditched the vegan diet for a mainly plant based with salmon/eggs/low histamine cheese) and have done my own research. I followed the plan of methionine (zinc methionine that also had b6), C, Magnesium and low histamine diet. I’ve stopped taking probiotics. Right now my b is too high 140 ug/L from the methionine supp. Need to find one where b6 is not included.
My main symptom now is runny nose. I have treated the insomnia with GABA and magnesium (CALM)
Does activated charcoal (coconut based) sop up extra histamine?
Do you have any suggestions? I’m starting to get frustrated at the slow pace.
Thank you,
Sam
My husband can’t function without daily anti-histamine drugs, namely Zyrtec. He’s been suffering terrible allergies all his life, and even with allergy shots he is still dependent on daily Zyrtec so it seems futile to order a whole blood histamine test since he can’t go off for a month duration. Does this pretty much mean that he is an under-methylator who needs to avoid folic acid? I recently gave him some organic celery juice (high in folate) and he definitely feels ill immediately after and did not feel well besides the juice causing acute diarrhea every single time. Within last few days, he’s been noticing muscle spasms and fatigue, and I’m trying to understand his methylation status especially because his stress/anxiety is sky high.
There’s a pretty good chance he’s an undermethylator. Best to test with another panel that is not affected by anti-histamines. This is the Methylation Panel by Doctor’s Data that measures SAMe, methionine, homocysteine, SAH and adenosine. That is the gold standard for methylation evaluation. But it is not a good test for overmethylators and it is not useful if someone has been taking SAMe and methionine.
Eosinophilia is commonly elevated with intestinal parasites. This is another pandemic that is hardly discussed. It does appear that you are undermethylated, though it is best to look at a history and review full Walsh Panel before treating. For instance treating methylation prior to proper evaluation of “plasma” zinc and copper overload status can be problematic. Some of the worst behavior disorders come from overmethylation (and overmethylating) plus elevated free copper. Suggest proper test of plasma zinc and then treat your copper overload, THEN work on methylation. Meantime, you’ll need a good natural protocol for intestinal parasites. These, worms in particular, are a major source of intestinal dysbiosis, skin rashes, back pain, sleep disorders, and mood problems.
How much SAMe and how much methionine is required for undermethylater with high histamine?
This depends on symptoms and weight, plus history and current medications. We don’t treat all undermethylators wwith SAMe, for instance Bipolar Disorder or those with high copper do not do well with SAMe or until copper and zinc levels are first corrected.
Hey thanks for your reply, and sorry for my delayed response. That makes sense, especially with SAM-e. But if one doesn’t have enough methylcobalamin or other methyl-groups, then I’m guessing methionine won’t work quite as well as SAM-e.