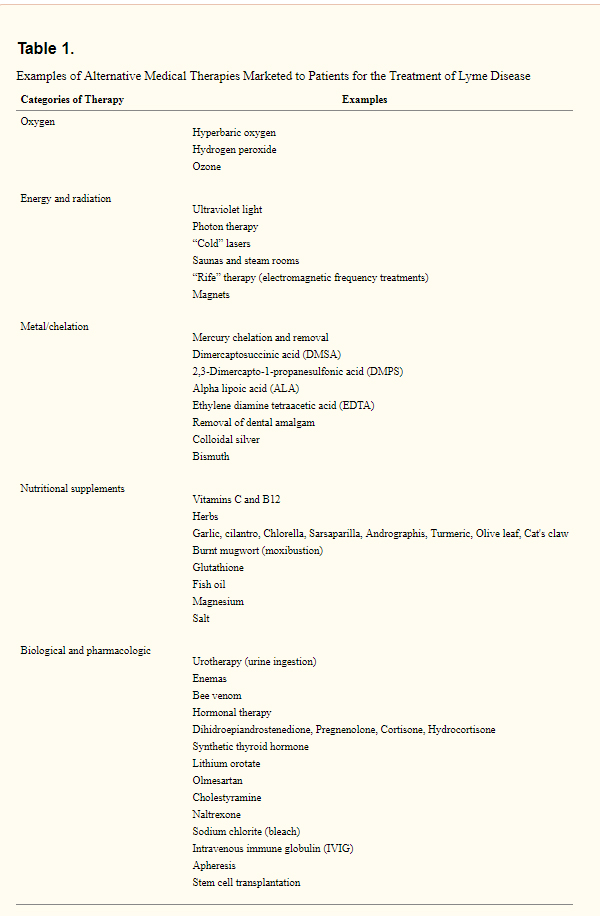
Understanding Lyme Disease, Biofilms, and New Treatment Approaches
What is Lyme Disease?
Lyme disease is an infectious illness caused by the Borrelia burgdorferi bacteria, primarily transmitted to humans through the bite of infected black-legged ticks (commonly called deer ticks). The disease is most prevalent in North America and parts of Europe, especially in forested or grassy areas where these ticks thrive. Early symptoms often include a bullseye-shaped rash (erythema migrans), flu-like symptoms such as fever, chills, and fatigue, as well as joint and muscle pain.
If untreated, Lyme disease can progress to more severe manifestations, including neurological problems (like facial paralysis and memory issues), heart rhythm irregularities, and long-term joint inflammation (Lyme arthritis). The severity of the disease varies greatly depending on how quickly it is diagnosed and treated.
Standard Treatment Options
In most cases, Lyme disease is treated with antibiotics like doxycycline, amoxicillin, or cefuroxime, which are effective when the disease is caught in its early stages. The standard course of antibiotics lasts two to four weeks, but in some cases, symptoms can persist after treatment—this is often referred to as Post-Treatment Lyme Disease Syndrome (PTLDS).
Persistent or chronic Lyme cases, where symptoms linger for months or years, are challenging to treat. This has led researchers and practitioners to explore additional therapies, including those targeting biofilms.
The Role of Biofilms in Lyme Disease
What Are Biofilms?
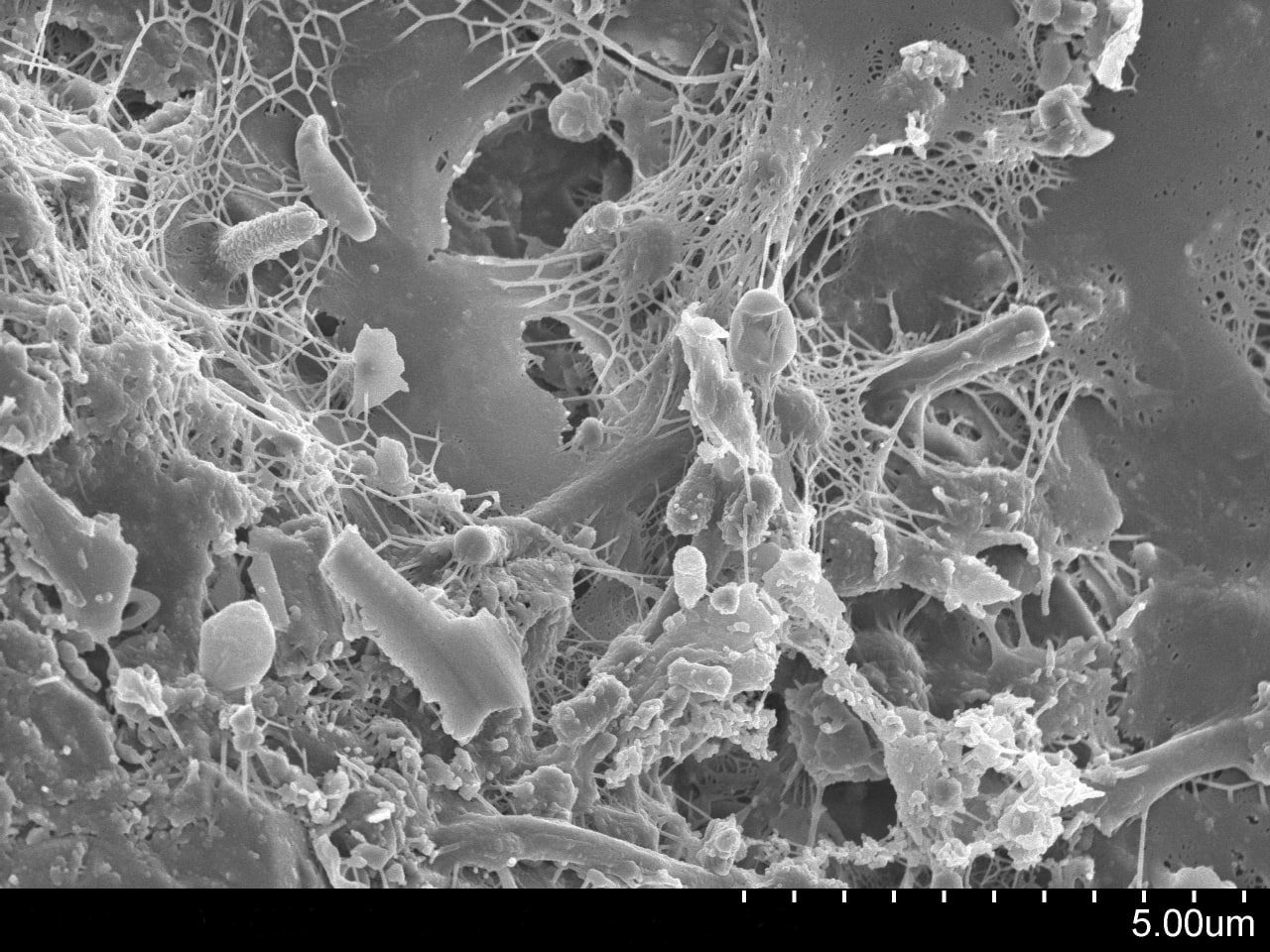
Biofilms are complex, sticky structures that bacteria form to protect themselves from hostile environments, including the human immune system and antibiotics. When Borrelia and other bacteria form biofilms, they create a matrix of slime, known as extracellular polymeric substance (EPS), which allows them to adhere to surfaces and grow as a community. This biofilm acts like a shield, making it harder for both the immune system and antibiotics to reach and kill the bacteria.
Studies have shown that Borrelia can form biofilms, and while biofilms may not be the primary mechanism of illness in Lyme disease, their presence may contribute to antibiotic resistance and chronic symptoms.
Biofilm Treatment Approaches
Given the difficulty in treating bacteria shielded by biofilms, newer treatment strategies are being explored, often in conjunction with standard antibiotic therapy.
- N-acetyl cysteine (NAC): NAC is commonly known to help break down mucus but may also play a role in dissolving biofilms. By reducing the protective matrix of the biofilm, NAC can potentially make the bacteria more susceptible to treatment.
- Enzymes: Digestive enzymes, such as serrapeptase or lumbrokinase, are thought to help dissolve biofilms, especially in the gut. These enzymes can break down the protein and sugar components of the biofilm, exposing the bacteria to the immune system and antibiotics.
- Oxygen Therapy: Oxygen, particularly in the form of hyperbaric oxygen therapy, has been studied as a way to break through biofilm barriers. Oxygen can penetrate deep into tissues and biofilms, helping to degrade the matrix and inhibit bacterial survival.
- Ozone Therapy: Dr. Frank Shallenberger, and Robert Rowan, MD, pioneers in ozone therapy, have suggested that ozone’s ability to increase oxygen delivery to tissues can help combat biofilms and boost the immune system's ability to fight infections. Ozone therapy introduces ozone into the body, which can improve blood oxygenation, enhance immune responses, and degrade harmful biofilms, allowing for better treatment outcomes. This is particularly promising for cases of chronic Lyme disease where biofilms may be playing a significant role.
- EDTA Chelation: EDTA is a chelating agent that binds to minerals like calcium, which are essential components of biofilms. By removing these minerals, EDTA can help break down biofilms, though care must be taken as it can also remove beneficial minerals from the body.
Diagnosis of Lyme Disease
These labs are most used for Lyme Disease Testing:
- Enzyme-Linked Immunosorbent Assay (ELISA): This is the standard first test, designed to detect antibodies against Borrelia burgdorferi. If positive, it indicates the presence of an immune response to the bacteria.
- Western Blot: Used as a confirmatory test following a positive ELISA, this detects specific proteins from Borrelia and helps distinguish between early and late-stage infection based on IgM and IgG antibodies.
- PCR (Polymerase Chain Reaction): This test looks for Borrelia DNA directly in samples like blood, cerebrospinal fluid, or joint fluid. PCR is more useful in later stages of the disease or in chronic cases where biofilms may be involved.
- Quorum Sensing and Biofilm Detection: While not part of the typical diagnostic panel, emerging research suggests that understanding bacterial communication (quorum sensing) and biofilm formation could lead to more targeted diagnostic tools in the future.
Integrating Biofilm Therapies with Lyme Disease Treatment
While Lyme disease is not primarily driven by biofilm formation, biofilms can complicate chronic Lyme cases by sheltering Borrelia from the immune system and antibiotics. Rowan and Shallenberger’s research on biofilm therapies, including the use of oxygen and ozone therapy, opens up promising treatment avenues. Integrating these therapies with traditional antibiotic treatment could help break down biofilms, enhance immune function, and improve recovery outcomes.
While antibiotics remain the cornerstone of Lyme disease treatment, addressing biofilms through therapies like NAC, enzymes, and ozone could provide a more comprehensive approach to managing chronic Lyme disease, reducing symptoms, and improving long-term recovery.
This is a 30 minute video with Dr. Alan MacDonald, a retired M.D. and board certified in Anatomic Pathology and Clinical Pathology.
This revealing interview from May 2013 (1 of 3) covers many of the controversies associated with
Lyme disease: - Chronic lyme disease; - Alzheimer's and Lyme disease: microscopy and culturing brain tissue; -
How Borrelia changes and survives within the human host; - The many strains and variations in Borrelia, how this relates to flawed testing. The complete interview is available from The Arthroplasty Patient Foundation. Contribute an any-sized donation (more if outside the U.S.) at this link:
https://www.arthropatient.org/about/do... Our specific library of current intelligence on biofilms:
Our documentary on biofilms, Why Am I Still Sick, now available in French, Spanish, Simplified and Traditional Chinese: