Copper Imbalance: Causes, Symptoms and Increasing Ceruloplasmin to Improve Free Copper
What is Ceruloplasmin?
Ceruloplasmin is a multi-copper oxidase enzyme that plays a crucial role in the transportation of copper throughout the body. It is synthesized in the liver and released into the bloodstream, where it binds to copper and transports it to the organs and tissues that require it. Ceruloplasmin has six copper atoms in its structure, and each copper atom can bind to copper ions, preventing them from being oxidized and damaging surrounding tissues.
Copper ions can easily become oxidized, and the resulting free radicals can cause significant damage to cells and tissues. When copper is bound to ceruloplasmin, it is protected from oxidation, and it can be safely transported to the organs and tissues that need it. However, if there is low ceruloplasmin, a dysfunction or or a relative deficiency in ceruloplasmin, unbound copper can accumulate in various organs, leading to toxicity and damage. This is referred to as elevated free copper, when ratio of ceruloplasmin to copper is low, particularly when there is a marked elevation in total copper.
The organs that are most affected by copper toxicity are the liver, brain, and kidneys. Unbound copper can accumulate in the liver, leading to liver damage, and in the brain, it can contribute to neurodegenerative disorders such as Alzheimer's disease. Elevated copper levels in the kidneys can cause damage to the tubules, leading to renal dysfunction.
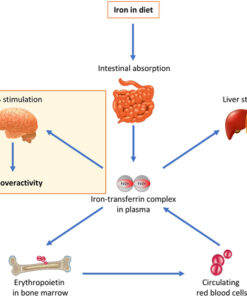
In addition to preventing copper from becoming oxidized, ceruloplasmin also plays a crucial role in the immune system. It can bind to and remove excess iron from the body, reducing the risk of iron overload and associated complications.
Importance of Raising Low Ceruloplasmin in Maintaining Copper Balance
Ceruloplasmin plays a crucial role in maintaining copper balance in the body. Copper is an essential mineral that is necessary for the proper functioning of enzymes and proteins involved in many physiological processes, including the production of energy, the formation of connective tissues, and the synthesis of neurotransmitters. However, excessive copper, particularly elevated free copper, can be toxic and damaging to cells and tissues, leading to a range of health problems. Ceruloplasmin helps to regulate copper levels in the body by binding with copper and carrying it safely to the liver, where it can be excreted or stored as needed.
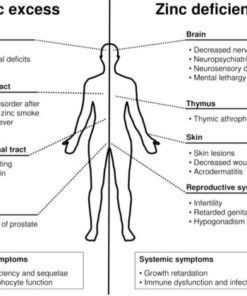
Copper bound to ceruloplasmin is less oxidizing and more stable than unbound copper. Unbound copper can generate reactive oxygen species (ROS) and cause oxidative damage to cells and tissues, leading to inflammation and tissue damage. This is especially problematic in organs that are rich in copper, such as the liver, brain, and kidneys. Elevated copper levels, which almost always accompanies a relatively low ceruloplasmin, can also impair the function of other minerals, such as zinc and iron, which are necessary for many physiological processes.
What is the Difference Between Ceruloplasmin and Metallothioneins?
Ceruloplasmin and metallothionein are two different proteins that are involved in copper regulation in the body.
Ceruloplasmin is a copper-containing protein that is produced in the liver and helps to transport copper in the blood. It plays a crucial role in maintaining the balance of copper in the body and protects against copper toxicity.
Metallothioneins, on the other hand, are a group of small, cysteine-rich proteins that are present in various tissues of the body, including the liver. They are able to bind to metals such as copper, zinc, and cadmium, and help to regulate their levels in the body. Metallothioneins are particularly important for binding excess copper and reducing the amount of free copper that is available in the body.
While ceruloplasmin and metallothionein both play important roles in copper regulation, they have different functions and mechanisms of action. Ceruloplasmin primarily helps to transport copper in the blood, while metallothioneins primarily bind to excess copper and reduce free copper levels in the body.
Ceruloplasmin and metallothionein levels may rise and fall together in response to certain stimuli such as copper and zinc status, inflammation, and oxidative stress. However, their functions and regulation are different. Ceruloplasmin mainly binds and transports copper in the blood, while metallothionein binds and regulates the levels of various metals including copper and zinc in the cells. Therefore, changes in one may not always reflect changes in the other.
Ceruloplasmin is typically used as a biomarker to evaluate copper overload because it is the main protein in the blood that binds and transports copper. It is relatively easy to measure ceruloplasmin levels in the blood, making it a convenient biomarker for copper status.
On the other hand, measuring metallothionein levels in the blood or tissues is more complex and less commonly used in clinical practice. Metallothionein is a small protein that can bind to various metals, including copper, zinc, and cadmium. However, measuring metallothionein levels can be challenging due to its low abundance in the body and its rapid turnover. Additionally, metallothionein levels can be influenced by a variety of factors, such as inflammation, oxidative stress, and exposure to certain metals.
In summary, while metallothionein can play a role in copper metabolism, ceruloplasmin is the more commonly used biomarker for evaluating copper overload.
Copper Toxicity and Depression and Anxiety
Studies have also found an association between copper toxicity and depression and anxiety. Copper is an essential micronutrient that plays a crucial role in various physiological processes, including the regulation of neurotransmitters and the immune system. However, elevated levels of copper can lead to oxidative stress, which can damage cells and tissues in the brain and other organs. In some individuals, copper toxicity can lead to psychiatric symptoms such as depression and anxiety.
Research has shown that individuals with depression and anxiety may have higher levels of copper in their blood, hair, and urine compared to healthy individuals. Additionally, studies have found that treating copper overload with chelation therapy can improve symptoms of depression and anxiety in some patients.
Role of Estrogen in the Activity of Copper and Ceruloplasmin
Estrogen plays a significant role in the activity of copper and ceruloplasmin. Estrogen increases the production of ceruloplasmin, which helps to transport copper in the blood. However, excessive estrogen can also cause copper levels to rise, leading to copper toxicity. This is because estrogen stimulates the production of proteins that bind copper, such as metallothionein. Metallothionein binds copper and can lead to an increase in unbound, toxic copper levels. Additionally, estrogen can increase the permeability of blood vessels, allowing copper to leak out of the bloodstream and accumulate in tissues.
Estrogen has been shown to increase metallothionein production in some tissues, which may lead to an increase in copper binding to metallothionein and a reduction in free copper. However, in other tissues such as the liver, estrogen can actually decrease metallothionein production and increase free copper levels. Additionally, estrogen can increase the amount of copper that is transported from the gut into the bloodstream, leading to an overall increase in copper levels in the body. So while estrogen may have some positive effects on copper regulation through metallothionein production, it can also have negative effects that lead to copper overload. The exact mechanisms are complex and may depend on various factors such as the type of tissue and the individual's overall health status.
Autistic children have a high prevalence of elevated free copper. High levels of estrogen, contributing to low ceruloplasmin is found to play a role in Autism Spectrum Disorder. Follow this link to see learn more about copper, estrogen and oxidative stress from vaccines may all be factors in Autism.
Genetic factors that can affect copper and ceruloplasmin levels
Mutations in the ATP7A and ATP7B genes can cause copper accumulation in various tissues and result in conditions such as Menkes disease and Wilson disease. These genes encode proteins involved in copper transport and metabolism, and mutations can affect their function. Other genetic factors, such as polymorphisms in genes related to copper homeostasis, may also contribute to individual differences in copper and ceruloplasmin levels.
In addition, genetic factors can interact with environmental factors, such as diet and exposure to toxins, to affect copper and ceruloplasmin levels. For example, some individuals may have a genetic predisposition to copper overload and be more susceptible to the effects of high copper intake from the diet. Understanding the genetic factors that contribute to copper and ceruloplasmin metabolism can be important for identifying individuals at risk for copper-related conditions and developing personalized approaches to prevention and treatment.
Digestive Health and Diet Effect on Ceruloplasmin Levels
Conditions such as yeast overgrowth, leaky gut, and dysbiosis can all contribute to impaired absorption of copper and other nutrients, leading to copper deficiency and decreased ceruloplasmin production. Moreover, poor dietary choices such as excessive consumption of sweets, carbohydrates, and processed foods can increase oxidative stress levels in the body, which can further decrease ceruloplasmin levels. Therefore, maintaining a healthy gut microbiome and consuming a balanced diet rich in essential nutrients is crucial for optimal copper metabolism and ceruloplasmin production.
Sulfur and the Important Amino Acids in Ceruloplasmin Production
Ceruloplasmin production requires several amino acids, including cysteine, histidine, and methionine. Cysteine is of particular importance as it provides the sulfur necessary for ceruloplasmin's enzymatic activity. Cysteine can be found in foods such as poultry, eggs, and legumes.
Supplementation with N-Acetyl-Cysteine (NAC) has been shown to increase cysteine levels and promote ceruloplasmin activity. Other sulfur-containing supplements such as alpha-lipoic acid and MSM (methylsulfonylmethane) may also be beneficial.
Minerals, vitamins, and amino acids that can help reduce oxidative stress from copper overload
- Zinc: plays a crucial role in balancing copper levels and preventing copper toxicity. It also acts as an antioxidant, protecting cells from oxidative stress.
- Selenium: an important mineral that is involved in the production of glutathione, a powerful antioxidant that helps protect against oxidative damage caused by copper overload.
- Manganese or Molybdenum: a trace mineral that is necessary for the production of the antioxidant enzyme superoxide dismutase (SOD), which helps protect against oxidative stress. However it is necessary to use caution with persons with low serotonin depression, Tic disorders, and with children when using manganese.
- Vitamin C: a powerful antioxidant that can help reduce oxidative stress caused by excess copper.
- Vitamin E: another potent antioxidant that can help protect against oxidative damage caused by copper toxicity.
- N-Acetyl-Cysteine (NAC): an amino acid that can help boost levels of glutathione, a potent antioxidant that helps protect against oxidative stress.
- Methionine: an essential amino acid that is necessary for the production of glutathione and other important antioxidants.
- Taurine: an amino acid that can help protect against oxidative stress and inflammation caused by copper overload.
Key nutrients to improve low ceruloplasmin levels
- Copper: despite its role in causing copper overload, copper is also necessary for the production of ceruloplasmin. If copper levels are too low, ceruloplasmin production can be affected.
- Zinc: as mentioned earlier, zinc plays a crucial role in balancing copper levels. It also helps increase the production of ceruloplasmin.
- Vitamin A: studies have shown that vitamin A can increase the activity of ceruloplasmin.
- Vitamin C: in addition to its antioxidant properties, vitamin C has been shown to increase the production of ceruloplasmin.
- Vitamin E: research suggests that vitamin E can help increase the activity of ceruloplasmin.
Biotype Nutrients is a nutritional supplements website developed by Second Opinion Physician. Click on the logo to find supplements for low ceruloplasmin and copper overload. Includes zinc piccolinate, alpha lipoic acid, selenium and antioxidant blends.
Understanding Copper Overload
Testing for Copper Overload
Other Single Item Tests
All Cognoscopy Labs
All Cognoscopy Labs
All Cognoscopy Labs
Walsh Approach Test Panels