OCD Methylation and Mitochondria: Ketone Ester Therapy & Metabolic Treatment
OCD methylation and mitochondria are deeply connected through energy-dependent methylation, glutamate regulation, and mitochondrial ATP production. Obsessive-compulsive symptoms, chronic rumination, cognitive rigidity, sensory overload, and trauma-linked looping behaviors are increasingly recognized as manifestations of deeper metabolic patterns involving methylation, mitochondrial function, and glutamate regulation. Traditional psychiatric models rarely address these pathways, yet clinical experience shows that many patients improve only when these biochemical foundations are treated directly.
This article outlines a comprehensive, metabolically informed approach that integrates methylation support, mitochondrial restoration, ketone ester therapy, creatine physiology, and glutamate/NMDA modulation. The model builds upon established principles from nutrient-based psychiatry while incorporating newer insights from metabolic neuroscience. Together, these components form a unified strategy for conditions where OCD-like symptoms, intrusive thoughts, attentional rigidity, and high stress reactivity dominate.
The Core Link: Undermethylation and Mitochondrial Dysfunction
A significant proportion of patients presenting with cognitive rigidity, looping thoughts, or internal tension show evidence of undermethylation and mitochondrial dysfunction. Methylation depends on adequate levels of methionine, SAM (S-adenosylmethionine), and critical cofactors — but its true limiting factor is ATP. The enzyme methionine adenosyltransferase requires ATP to convert methionine into SAM. When mitochondria under-produce ATP, SAM levels fall and methylation bottlenecks develop.
This explains why mitochondrial dysfunction symptoms — fatigue, cognitive slowdown, dysautonomia, heat intolerance, tremors, or sensory overload — often parallel the emotional and cognitive patterns seen in undermethylation. It also aligns with SAMe deficiency symptoms such as poor stress tolerance, mood rigidity, and slow emotional recovery. The overlap between undermethylation and mitochondrial impairment forms the foundational biochemical signature seen in many individuals with chronic cognitive rigidity.
Undermethylation as the Biochemical Foundation for OCD
Among individuals with obsessive thinking patterns, one of the clearest biochemical contributors is the link between OCD and undermethylation. When SAM levels are low, the brain’s capacity for neuroplasticity decreases. This affects synaptic pruning, neurotransmitter turnover, and emotional reset pathways.
Patients whose OCD patterns stem from undermethylation describe:
-
thoughts that “stick” or replay persistently
-
difficulty letting go of intrusive worries
-
perfectionistic control strategies
-
heightened internal tension
-
poor response to SSRIs
-
sensitivity to stress and novelty
These features make metabolic treatment for OCD an essential consideration. When undermethylation coexists with insufficient ATP, interventions that address only neurotransmitters fail to resolve the deeper biochemical patterns preventing cognitive flexibility and adaptive emotional processing.
NMDA Receptors, Glutamate, and the OCD Loop
Glutamate is the brain’s primary excitatory neurotransmitter, and NMDA receptors play a central role in learning, memory, sensory processing, and emotional adaptation. In many patients with OCD-like patterns, OCD and elevated NMDAR activity maintain a state of hyperarousal and overactivation within cortico-striatal loops.
When mitochondrial function is impaired, astrocytes struggle to clear glutamate effectively. This produces glutamate sensitivity symptoms, including:
-
heightened sensory awareness
-
agitation
-
emotional lability
-
insomnia
-
stress-triggered cognitive freezing
-
amplification of intrusive thoughts
Glutamate excess disrupts extinction learning — the ability to update or erase old threat associations. This is why OCD persists: the brain cannot fully encode “nothing is wrong.” The combination of glutamate overload, NMDA hyperactivation, and low SAM establishes a cycle that continuously reinforces intrusive thinking and rigid behavior patterns.
Mitochondria as the “Silver Bullet” in OCD and Cognitive Rigidity
Mitochondria power nearly every neurobiological process involved in emotional regulation, sensory processing, and cognitive control. When mitochondria falter, both methylation and glutamate balance suffer. This makes undermethylation and mitochondrial dysfunction a potent driver of psychiatric and neurological symptoms.
Clinically, mitochondrial dysfunction symptoms include:
-
dysautonomia (orthostasis, heat intolerance, POTS-like symptoms)
-
muscle rigidity or tremors
-
variable energy levels
-
cognitive fog
-
heightened reactivity to stress
-
worsening symptoms during infection or inflammation
-
poor exercise tolerance
These same patterns appear in Parkinson’s disease, neurodegenerative disorders, dysautonomia, and trauma-linked hyperarousal. The overlap highlights why metabolic treatment for OCD can have broader benefits across neurological and autonomic disorders.
Ketone Esters and Mitochondria: Restoring ATP and Glutamate Balance
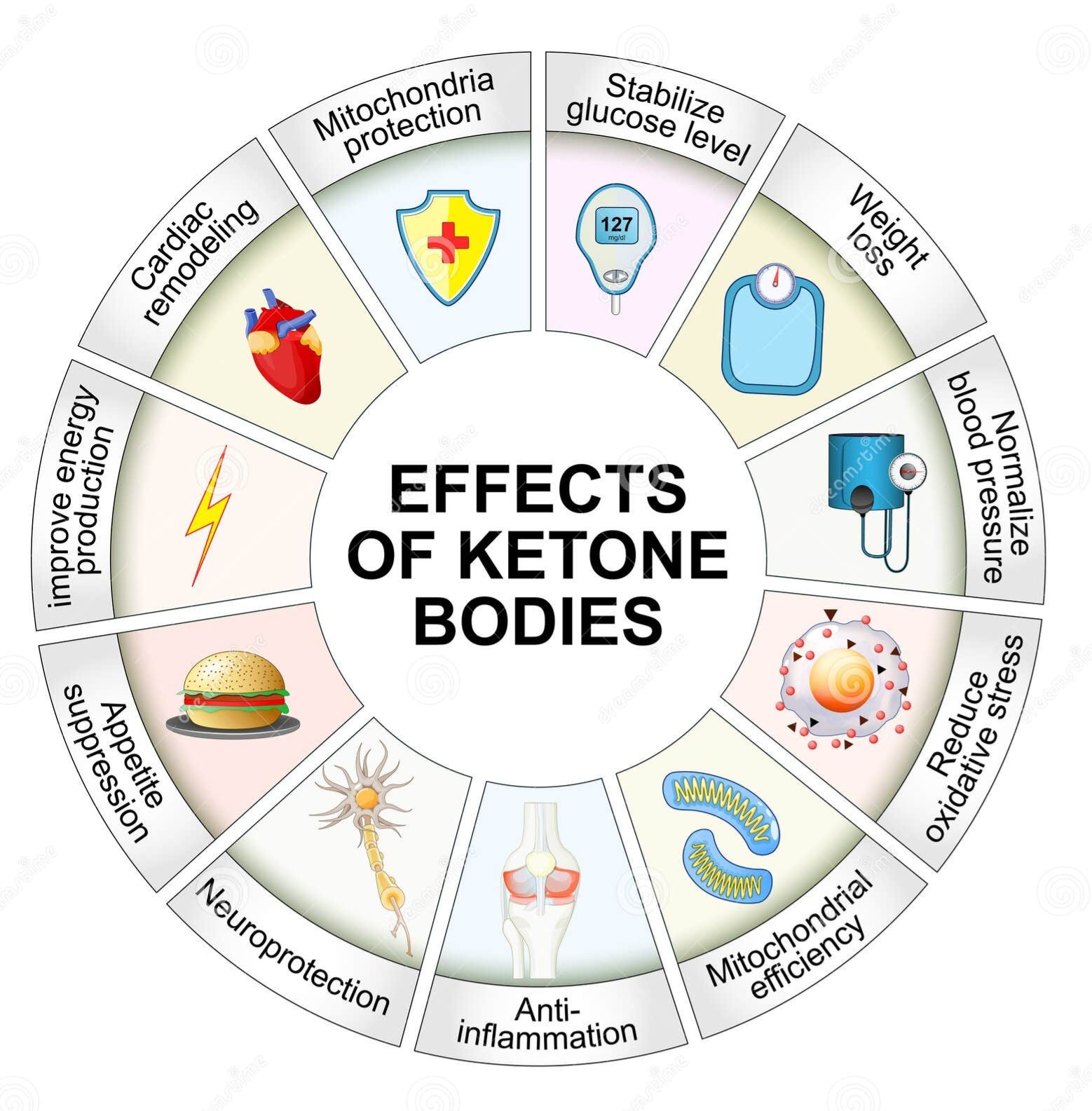
Ketone ester therapy addresses mitochondrial insufficiency by supplying beta-hydroxybutyrate (BHB), a high-efficiency fuel that produces more ATP per oxygen molecule than glucose. This makes ketone esters and mitochondria a powerful therapeutic pair, especially for individuals whose brain energy deficits contribute to cognitive rigidity and glutamate imbalance.
Ketones:
-
rapidly increase ATP availability
-
improve NAD⁺/NADH ratio
-
reduce oxidative stress
-
stabilize mitochondrial membrane potential
-
reduce glutamate release
-
support astrocytic glutamate recycling
These effects directly improve ketone supplements for brain function, especially in individuals with metabolic vulnerability, trauma history, or chronic neuroinflammation. Ketone esters help interrupt the energy-glutamate loop that drives OCD-like symptoms and restore conditions necessary for neuroplasticity and balanced emotional processing.
Ketone-based metabolic therapy is also being explored in cancer (as documented by Seyfried) because it supports healthy cell metabolism while selectively impairing cancer cell bioenergetics.
Ketone Esters and Brain Health: Supporting Methylation and Neuroplasticity
The relationship between ketone esters and brain health is especially important for undermethylated individuals. Because ketones provide a more efficient energy substrate, they support ATP production required for SAM synthesis. This enhances methylation capacity and improves the brain’s ability to shift out of rigid cognitive and emotional states.
Ketones also:
-
lower neuronal inflammation
-
improve signaling stability
-
enhance clearance of metabolic byproducts
-
reduce the “background noise” that drives sensory and emotional overload
This explains why many individuals with undermethylation, trauma loops, or sensory amplification experience improved calm, clarity, and adaptability when ketone ester therapy is added to their regimen.
Creatine, Phosphocreatine, and High-Demand Brains
Creatine plays a unique role in buffering brain energy, particularly in high-demand circuits responsible for working memory, inhibition, and emotional regulation. Deficiency or insufficient supply increases metabolic pressure on methylation since creatine synthesis consumes methyl groups.
This is why mitochondrial dysfunction symptoms such as tension, tremors, and cognitive fatigue often respond well to creatine. It also helps reduce glutamate sensitivity symptoms by stabilizing neuronal energy supply and reducing excitotoxic stress.
Patients who benefit from creatine often show:
-
high internal tension
-
muscle or motor rigidity
-
trauma-linked hypervigilance
-
sensory-driven exhaustion
-
high catecholamine turnover
-
chronic fatigue
-
difficulty with sustained cognitive effort
Creatine relieves metabolic bottlenecks, allowing methylation to operate more efficiently.
Mitochondrial Cofactor Therapy
A comprehensive metabolic strategy includes nutrients that support mitochondrial repair and redox balance:
-
Magnesium – stabilizes NMDA receptors
-
CoQ10 – supports the electron transport chain
-
Alpha-lipoic acid (ALA) – enhances mitochondrial redox cycling
-
Taurine – regulates calcium and inhibitory tone
-
Carnitine – transports fatty acids into mitochondria
-
NAC – boosts glutathione for detoxification and oxidative stress control
These cofactors complement mitochondrial repair and enhance metabolic treatment for OCD by improving energy availability and reducing excitatory overload.
Methylation Support Guided by Plasma or DD Testing
Effective methylation support begins with clear data. DD methylation analysis or plasma methionine/SAM/SAH panels reveal:
-
methylation efficiency
-
SAM/SAH ratio
-
methionine sufficiency
-
oxidative stress burden
-
zinc/copper ratios
-
presence of inflammation affecting the methylation cycle
Treatment may include:
-
methylcobalamin
-
methylfolate (in appropriate cases)
-
P5P
-
TMG or betaine
-
methionine support
-
zinc correction
-
gentle titration of SAMe
Because undermethylation is closely linked to OCD-like presentations, supporting methylation improves OCD and undermethylation symptoms when paired with mitochondrial stabilization.
Diet, Glutamate Reduction, and Circadian Repair
Nutrition and lifestyle patterns exert powerful effects on glutamate balance and mitochondrial health. Patients with glutamate sensitivity symptoms often improve by reducing intake of high-glutamate foods such as:
-
aged cheeses
-
soy
-
MSG-rich foods
-
heavily processed broths
-
processed meats
Glycemic stabilization prevents fluctuations in mitochondrial function and reduces excitatory neurotransmission. Anti-inflammatory diets further reduce oxidative stress, which is a driver of OCD glutamate imbalance and NMDA receptor instability.
Circadian repair — consistent sleep timing, light exposure, and autonomic stabilization — further enhances mitochondrial recovery.
Integrating All Components: A Unified Metabolic Treatment for OCD
The relationship between OCD and elevated NMDAR activity and mitochondrial impairment becomes clear when viewed through this metabolic lens. Elevating ATP through ketone therapy and targeted nutrients improves methylation, reduces glutamate toxicity, and stabilizes emotional circuitry. This is why combining methylation support with ketone esters and mitochondria-focused interventions offers transformative outcomes.
The same metabolic signature appears in:
-
Parkinson’s disease
-
neurodegenerative disorders
-
dysautonomia
-
chronic infections
-
metabolic cancer biology
These all share mitochondrial vulnerability as a core feature.
Summary and Clinical Roadmap
This integrated model identifies the central role of OCD and undermethylation in cognitive rigidity and intrusive thoughts, emphasizing that these patterns are amplified by undermethylation and mitochondrial dysfunction. Restoring ATP production, improving methylation capacity, lowering glutamate toxicity, and enhancing neuroplasticity form the foundation of a comprehensive metabolic plan.
Ketone esters, creatine, mitochondrial cofactors, and targeted methylation support work together to stabilize the brain’s energy systems, reduce excitotoxicity, and improve cognitive and emotional flexibility. This unified metabolic strategy provides a pathway for symptom improvement in complex cases where traditional psychiatric treatments fall short.
Research & References
-
SAM synthesis and ATP dependence: https://doi.org/10.1074/jbc.M110.212696
-
Ketones and NAD⁺ enhancement: https://doi.org/10.1016/j.cmet.2018.05.016
-
Glutamate in OCD: https://doi.org/10.1016/j.biopsych.2010.03.009
-
Extinction learning and NMDA: https://doi.org/10.1038/nrn1535
-
Ketone esters and cognitive function: https://doi.org/10.1152/japplphysiol.00717.2011
-
Cancer as a metabolic disease: https://doi.org/10.1002/cncr.27697
-
ALA/carnitine and mitochondrial repair: https://doi.org/10.1073/pnas.91.8.3265
Call to Action
If you struggle with intrusive thoughts, rigid thinking patterns, chronic anxiety, sensory overload, or symptoms that worsen under stress, these may reflect deeper metabolic pathways involving methylation and mitochondrial function.
A structured evaluation can clarify your biochemical profile and guide a personalized metabolic plan that supports brain energy, emotional regulation, and cognitive flexibility.
Begin your assessment with Second Opinion Physician and explore a metabolic approach to OCD and related symptoms.
