SECOND OPINION SERIES
Ketones Not Glucose: The Metabolic Mechanism Behind Ketogenic Therapy for OCD
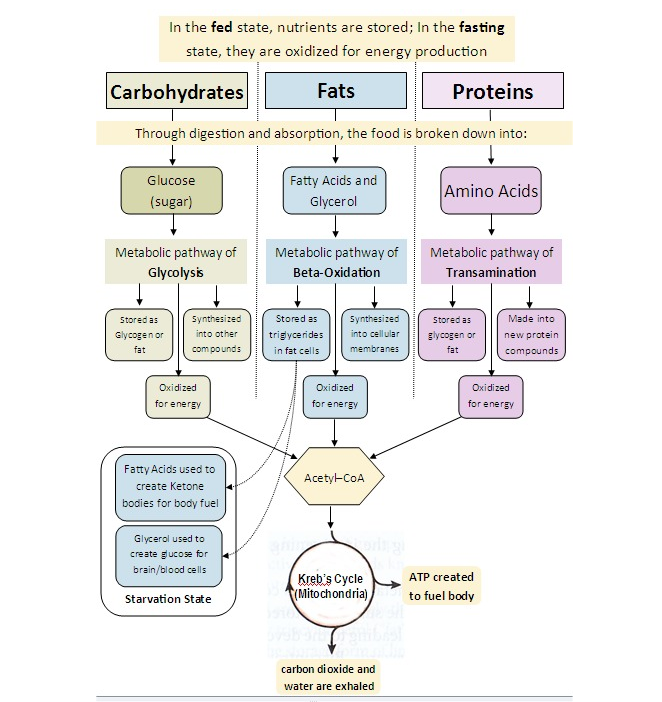
Many patients exploring ketogenic therapy for OCD want to understand why ketones calm intrusive thoughts while glucose metabolism often worsens them. The answer comes down to metabolic demand, oxidative stress, neurotransmitter balance, and inflammatory signaling. When the brain runs on ketones—not glucose—it becomes more efficient, less inflamed, and far less reactive to glutamate-driven electrical pressure. This shift is central to ketogenic therapy for mental health and explains why ketone ester therapy often produces rapid symptom relief.
Patients repeatedly describe the same transformation:
“The static went away.”
“My brain wasn’t scanning for danger.”
“I felt calm without feeling sedated.”
Below, I explain the biochemistry of ketones vs glucose, how this influences NMDAR activity, and why ketogenic therapy for inflammation is now being studied in OCD, anxiety, trauma, and neurodegenerative disorders.
Why Glucose Metabolism Can Increase OCD Symptoms
Glucose is a fast, glycolysis-driven fuel that produces more metabolic waste, more reactive oxygen species (ROS), and more excitatory neurotransmission. For a glutamate-sensitive brain, this is a problem. Individuals with undermethylation, copper overload, inflammation, or mitochondrial dysfunction are especially vulnerable to glucose-induced excitatory pressure.
Expanded clinical explanation:
-
Glucose increases glutamate release under physical or emotional stress, directly fueling intrusive thoughts.
-
Glycolysis produces more oxidative stress, which further amplifies NMDAR activity.
-
Mitochondria work harder, leading to energy crashes that destabilize mood and impulse control.
-
Glucose swings disrupt CSTC loop regulation, making “sticky thoughts” more persistent.
-
Glucose amplifies norepinephrine, increasing urgency, fear, and compulsive drive.
This is why patients often experience OCD flares after sugar, refined carbohydrates, restaurant meals, or high-stress days. Glucose metabolism excites the very circuits that OCD patients struggle to regulate.
When taken together, glucose mechanisms create the “perfect storm” that ketogenic therapy aims to calm.
Why the Brain Performs Differently on Ketones
When the body shifts to ketones not glucose, the entire neurochemical landscape changes. Ketones produce more ATP per unit oxygen, generate fewer free radicals, and directly regulate excitatory pathways that drive OCD symptoms.
Expanded mechanisms of ketone-based stability:
-
Ketones reduce glutamate release and prevent overstimulation of CSTC circuits.
-
NMDAR activity decreases, lowering intrusive thought intensity.
-
GABA tone increases, promoting calm, focused stability.
-
Microglia quiet down, reducing inflammatory glutamate release.
-
Mitochondrial function improves, enhancing cognitive endurance and emotional resilience.
-
Blood sugar becomes stable, removing glucose-driven anxiety spikes.
This is the foundation of ketogenic therapy for mental health: it restores metabolic calm to an overly reactive system.
Patients describe it as:
“My thoughts stopped shouting. They talked instead.”
Biochemistry of Ketones vs Glucose: Why Fuel Choice Changes Brain Chemistry
This section uses the planned SEO synonyms:
✔ biochemistry of ketones vs glucose
✔ metabolism of ketones versus glucose
Glucose Metabolism → High-Stress Fuel
-
Produces more ROS → oxidative stress → NMDAR sensitization
-
Increases intracellular calcium → excitotoxic pressure
-
Elevates glutamate release → more intrusive thought loops
-
Causes rapid ATP fluctuations → poor inhibitory control
-
Activates microglia → inflammation → compulsive cycles
For patients with undermethylation, copper overload, or low zinc, glucose metabolism is uniquely destabilizing.
Ketone Metabolism → Low-Stress Fuel
-
Generates fewer ROS → calmer NMDAR activity
-
Increases mitochondrial efficiency → more stable cognition
-
Reduces glutamate release → interrupts OCD loops
-
Enhances GABA pathways → better impulse control
-
Lowers inflammation → reduces biochemical triggers
-
Supports phospholipid synthesis → stabilizes membranes
This is why metabolism of ketones versus glucose is central to the success of ketogenic therapies across psychiatric conditions.
Ketogenic Therapy for Inflammation (and Why OCD Improves When Inflammation Falls)
Inflammation is one of the strongest drivers of glutamate toxicity and NMDAR hyperactivity. For patients with PANS/PANDAS, mold toxicity, Lyme, or chronic infections, inflammatory flare-ups directly worsen intrusive thoughts.
Expanded science:
-
IL-6 and TNF-α increase NMDAR phosphorylation, making neurons hypersensitive.
-
Microglia release glutamate when activated, worsening ruminative thought patterns.
-
Inflammation weakens GABAergic tone, removing inhibitory brakes.
-
High oxidative stress increases extracellular glutamate, increasing looping thoughts.
-
Copper dysregulation worsens inflammation, creating a feedback loop.
This is why ketogenic therapy for inflammation improves OCD symptoms: ketones reduce neuroinflammation by 20–40% in imaging studies, independent of diet quality.
Ketogenic Therapy for Mental Health: Why It Works Beyond OCD
Although this article focuses on ketogenic therapy for OCD, the same mechanisms apply broadly across mood and anxiety disorders.
Benefits observed in mental health populations:
-
Improved emotional resilience
-
Fewer intrusive memories
-
Better sleep architecture
-
Reduced amygdala hyperactivation
-
Greater mood stability
-
Improved cognitive switching
-
Reduced agitation during stress
Recent and accumulating studies on humans and animal models have shown that KD is beneficial to neurodegenerative diseases through modulating central and peripheral metabolism, mitochondrial function, inflammation, oxidative stress, autophagy, and the gut microbiome.
Ketone Ester Therapy: Fast-Acting Alternative to a Strict Ketogenic Diet
Dietary ketosis takes time and is difficult for many patients with anxiety and executive-function challenges. Ketone ester therapy bypasses these limitations by raising blood ketones within 15–30 minutes.
Expanded mechanisms:
-
Immediate reduction in NMDAR firing rate
-
Drop in glutamate release and synaptic spillover
-
Stabilization of mitochondrial membrane potential
-
Reduction in inflammatory cytokines (IL-1β, IL-6)
-
Increased BDNF signaling → improved cognitive flexibility
-
Rapid GABA upregulation → reduced sensory overload
Patients frequently notice:
“My brain quieted in 20 minutes.”
“My compulsions felt less urgent.”
“I didn’t react the same way to triggers.”
This is the role of ketone ester therapy—a shortcut to the biochemical benefits of full ketosis.
