SECOND OPINION SERIES
Histamine Intolerance and Mental Health
Causes, Depression, and Natural Treatment Through Gut and Methylation Support
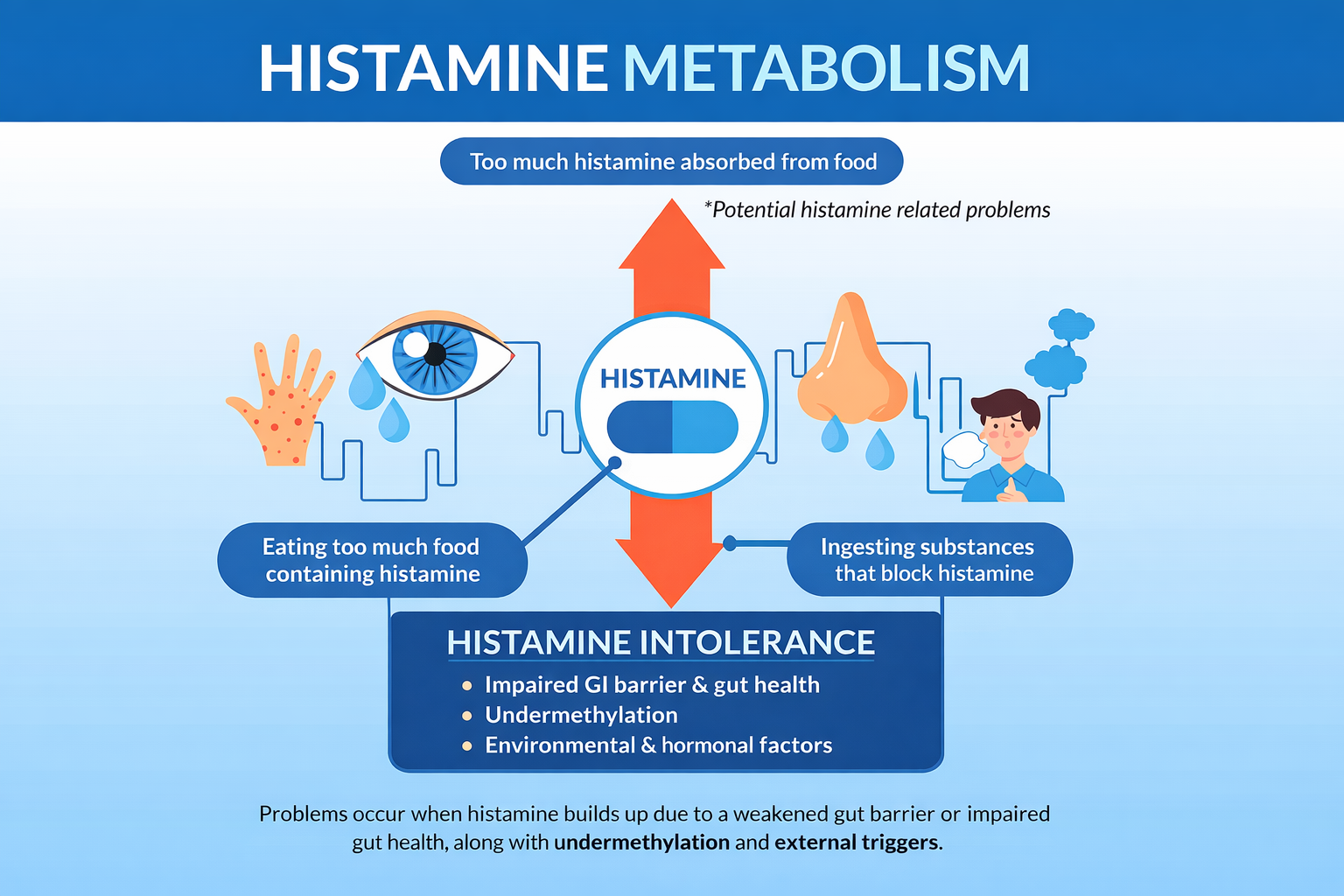
Histamine intolerance and mental health symptoms are closely linked, yet this connection is routinely misunderstood. Many patients struggling with anxiety, depression, OCD traits, irritability, insomnia, or emotional reactivity are told they have a “chemical imbalance,” when in reality they are experiencing histamine-driven neuroinflammation combined with impaired histamine clearance.

This article explains what histamine intolerance really is, the most common histamine intolerance causes, how histamine and depression are connected, and why natural treatment for histamine intolerance must address gut health, methylation status, and environmental triggers—not just symptoms. Particular attention is given to undermethylation and histamine, a pattern frequently seen in patients with persistent mental health symptoms.
What Is Histamine Intolerance?
Histamine intolerance is not a food allergy and not simply a reaction to “high-histamine foods.” It is a state in which histamine accumulates faster than the body can break it down, leading to systemic and neurological symptoms.
Histamine acts as:
-
A neurotransmitter in the brain
-
An immune signaling molecule
-
A regulator of stomach acid and gut motility
When histamine clearance fails, symptoms extend far beyond flushing or headaches and often manifest as psychiatric and cognitive disturbances.
Histamine Intolerance Causes
Understanding histamine intolerance causes is essential before choosing treatment. In most patients, histamine overload results from multiple converging factors, not a single defect.
Common causes of histamine intolerance include:
-
Impaired DAO (diamine oxidase) activity, the enzyme responsible for breaking down histamine in the gut
-
Gut inflammation or leaky gut, which increases histamine absorption
-
Dysbiosis, particularly bacteria that produce histamine
-
Nutrient deficiencies, especially vitamin B6, zinc, and copper imbalance
-
Chronic stress and cortisol dysregulation
-
Estrogen dominance, which slows histamine clearance
-
Environmental triggers, including mold, chemicals, and allergens
Many patients labeled with “histamine intolerance” are actually experiencing histamine overproduction combined with impaired clearance, which requires a broader clinical approach.
Histamine and Depression: The Overlooked Connection
The relationship between histamine and depression is often missed because histamine-driven depression does not resemble classic low-energy depression.
High histamine states are associated with:
-
Inner tension rather than emotional flatness
-
Anxiety, agitation, or obsessive thinking
-
Poor sleep with racing thoughts
-
Heightened sensitivity to noise, light, or stress
Histamine stimulates the brain and increases glutamate signaling. When histamine remains elevated, it contributes to NMDA receptor overactivity, neuroinflammation, and impaired serotonin function—not necessarily low serotonin production, but poor serotonin signaling and utilization.
This explains why many patients with histamine-related depression:
-
Worsen on SSRIs
-
Feel emotionally “wired but tired”
-
Experience paradoxical reactions to psychiatric medications
In these cases, treating histamine imbalance is often more effective than escalating antidepressant therapy.
Undermethylation and Histamine
Undermethylation and histamine are tightly linked in the Walsh model. Histamine serves as a functional biomarker of methylation status.
When methylation is insufficient:
-
Histamine breakdown slows
-
Histamine accumulates in the brain
-
Serotonin and dopamine signaling becomes dysregulated
Patients with undermethylation and high histamine often exhibit:
-
Depression with anxiety or irritability
-
OCD tendencies or rigid thinking
-
Seasonal worsening of symptoms
-
Sensitivity to folate or methyl donors if used incorrectly
Does SAMe or methionine help?
Sometimes—but only when used carefully. Supporting methylation without addressing gut inflammation or nutrient imbalances can temporarily worsen symptoms. Methylation support must be individualized and sequenced correctly.
Natural Treatment for Histamine Intolerance
(Gut Health, Diet, and Methylation First)
A natural treatment for histamine intolerance must address root causes, not merely suppress histamine receptors.
1. Gut Health Is the Foundation
The gut is the primary site of histamine breakdown. If the gut lining is inflamed or permeable, histamine intolerance will persist regardless of supplements.
Key priorities:
-
Heal intestinal permeability
-
Reduce inflammatory and allergenic foods
-
Correct dysbiosis
-
Support digestive enzyme function
2. Diet for Histamine Intolerance
A low-histamine diet alone is rarely sufficient, but diet matters.
Common dietary contributors:
-
Fermented foods
-
Aged cheeses
-
Processed meats
-
Alcohol
-
Food additives and preservatives
The goal is not lifelong restriction but reducing histamine burden while healing gut function.
3. Nutrient and Methylation Support
Effective natural treatment for histamine intolerance often includes:
-
Vitamin B6 (DAO activation)
-
Zinc (gut integrity and immune regulation)
-
Copper balance (not excess)
-
Carefully dosed methylation support when indicated
DAO and LDN: Helpful but Not Sufficient
DAO supplements
DAO can reduce acute food-related symptoms but does not correct histamine overproduction or gut inflammation. It is a tool, not a solution.
Low Dose Naltrexone (LDN)
LDN may help by:
-
Modulating immune activity
-
Reducing neuroinflammation
-
Supporting gut immune balance
However, LDN does not:
-
Heal leaky gut
-
Correct nutrient deficiencies
-
Restore methylation balance
For most patients, DAO or LDN alone is insufficient.
Is It Histamine Intolerance or High Histamine?
This distinction matters.
-
Histamine intolerance implies impaired breakdown
-
High histamine states may involve overproduction, mast cell activation, or inflammation
Clues suggesting high histamine rather than simple intolerance:
-
Symptoms unrelated to meals
-
Nighttime anxiety or insomnia
-
Sensory overstimulation
-
Worsening with stress or hormonal shifts
Clinical pattern recognition often matters more than isolated lab values.
When Depression Is the Primary Complaint
If depression is the dominant symptom:
-
Evaluate histamine status before escalating antidepressants
-
Assess methylation balance
-
Address inflammatory drivers
Treating histamine imbalance often improves mood, cognition, and sleep without increasing psychiatric medication burden.
Environmental and Lifestyle Drivers of Histamine
Even optimal nutrition fails if environmental triggers persist.
Common aggravators include:
-
Mold exposure
-
VOCs and fragrances
-
Chronic sleep deprivation
-
Psychological stress
-
Estrogen imbalance
Reducing environmental histamine load is often a turning point for resistant cases.
Moving Beyond Histamine Intolerance
True resolution occurs when:
-
Gut integrity is restored
-
Inflammatory foods are reduced
-
Methylation is stabilized
-
Environmental triggers are addressed
Histamine intolerance and mental health symptoms are not separate problems—they are interconnected expressions of biochemical imbalance.
Second Opinion Guidance
If you suspect histamine intolerance, undermethylation, or histamine-related depression may be contributing to persistent mental health symptoms, a structured, lab-guided evaluation can help clarify the underlying pattern and guide appropriate treatment.
Natural Treatment for Histamine Intolerance
(Gut Health, Diet, and Methylation First)
A natural treatment for histamine intolerance must address root causes, not merely suppress histamine receptors.
1. Gut Health Is the Foundation
The gut is the primary site of histamine breakdown. If the gut lining is inflamed or permeable, histamine intolerance will persist regardless of supplements.
Key priorities:
-
Heal intestinal permeability
-
Reduce inflammatory and allergenic foods
-
Correct dysbiosis
-
Support digestive enzyme function
2. Diet for Histamine Intolerance
A low-histamine diet alone is rarely sufficient, but diet matters.
Common dietary contributors:
-
Fermented foods
-
Aged cheeses
-
Processed meats
-
Alcohol
-
Food additives and preservatives
The goal is not lifelong restriction but reducing histamine burden while healing gut function.
3. Nutrient and Methylation Support
Effective natural treatment for histamine intolerance often includes:
-
Vitamin B6 (DAO activation)
-
Zinc (gut integrity and immune regulation)
-
Copper balance (not excess)
-
Carefully dosed methylation support when indicated
DAO and LDN: Helpful but Not Sufficient
DAO supplements
DAO can reduce acute food-related symptoms but does not correct histamine overproduction or gut inflammation. It is a tool, not a solution.
Low Dose Naltrexone (LDN)
LDN may help by:
-
Modulating immune activity
-
Reducing neuroinflammation
-
Supporting gut immune balance
However, LDN does not:
-
Heal leaky gut
-
Correct nutrient deficiencies
-
Restore methylation balance
For most patients, DAO or LDN alone is insufficient.
Is It Histamine Intolerance or High Histamine?
This distinction matters.
-
Histamine intolerance implies impaired breakdown
-
High histamine states may involve overproduction, mast cell activation, or inflammation
Clues suggesting high histamine rather than simple intolerance:
-
Symptoms unrelated to meals
-
Nighttime anxiety or insomnia
-
Sensory overstimulation
-
Worsening with stress or hormonal shifts
Clinical pattern recognition often matters more than isolated lab values.
When Depression Is the Primary Complaint
If depression is the dominant symptom:
-
Evaluate histamine status before escalating antidepressants
-
Assess methylation balance
-
Address inflammatory drivers
Treating histamine imbalance often improves mood, cognition, and sleep without increasing psychiatric medication burden.
Environmental and Lifestyle Drivers of Histamine
Even optimal nutrition fails if environmental triggers persist.
Common aggravators include:
-
Mold exposure
-
VOCs and fragrances
-
Chronic sleep deprivation
-
Psychological stress
-
Estrogen imbalance
Reducing environmental histamine load is often a turning point for resistant cases.
Moving Beyond Histamine Intolerance
True resolution occurs when:
-
Gut integrity is restored
-
Inflammatory foods are reduced
-
Methylation is stabilized
-
Environmental triggers are addressed
Histamine intolerance and mental health symptoms are not separate problems—they are interconnected expressions of biochemical imbalance.
Second Opinion Guidance
If you suspect histamine intolerance, undermethylation, or histamine-related depression may be contributing to persistent mental health symptoms, a structured, lab-guided evaluation can help clarify the underlying pattern and guide appropriate treatment.
