Natural Treatments for OCD That Calm an Overactive Brain
Many patients search for natural treatments for OCD because their symptoms feel mechanical, intrusive, and out of their control. What they often describe—racing thoughts, looping behaviors, emotional pressure, and sleep disturbance—matches a biochemical pattern involving glutamate signaling and NMDA receptor overactivity. In the Second Opinion Series, Dr. Epstein explains how patterns of glutamate and OCD interact, why an overactive brain OCD pattern feels so relentless, and how targeted nutrient and functional strategies can help.
This article clarifies these mechanisms in plain language. Below the introductory explanations, a deeper scientific section is included for readers who want the full neurochemical perspective.
What Symptoms of OCD Look Like When Glutamate Is Elevated
People often ask what actually drives the symptoms of OCD—is it personality, overthinking, or stress? In many cases, the underlying physiology is a persistent excitatory drive in the brain. When NMDA receptor activation runs too high, the neural circuits responsible for filtering thoughts become overloaded.
Patients describe:
-
rigid or repetitive thinking
-
intrusive thoughts that “grab hold”
-
difficulty shifting attention
-
nighttime mental restlessness
-
muscle tension or internal pressure
This helps explain why natural treatments for OCD frequently focus on calming overactive glutamate pathways, improving sleep, regulating methylation, and restoring antioxidant capacity.
How a Functional Medicine Doctor Understands Glutamate and OCD
From a functional medicine viewpoint, glutamate and OCD patterns rarely occur in isolation. They often emerge alongside:
-
undermethylation
-
elevated histamine
-
oxidative stress
-
low magnesium
-
poor antioxidant capacity
-
high homocysteine
-
chronic inflammation
These biochemical signatures promote NMDA overactivity, creating the overactive brain OCD experience patients describe as “always on.”
A natural approach aims to:
-
reduce excitatory pressure
-
stabilize glutamate-GABA balance
-
support methylation
-
improve sleep quality
-
restore antioxidant defenses
Understanding that these symptoms of OCD reflect measurable patterns—not character flaws—helps patients engage meaningfully with their treatment.
Why an Overactive Brain OCD Pattern Creates Thought Loops
Thought loops occur when NMDA and glutamate activity stay too high for too long, pushing circuits in the striatum and prefrontal cortex into repetitive cycles. This creates the classic sensation of intrusive thoughts that feel involuntary.
This explains why natural treatments for OCD often show benefit even when standard medications have been insufficient. They target the biochemical drivers instead of only the serotonin pathway.
When NMDA Receptor Overactivity Happens

When NMDA signaling is excessive:
-
neurons fire too easily
-
the brain stays in a “high-alert” mode
-
intrusive thoughts accelerate
-
mental tension increases
-
emotional regulation weakens
-
sleep becomes disrupted
This is the same excitatory pattern found in many glutamate and OCD presentations.
Consequences of Excessive NMDA Activity
People with elevated NMDA activity may experience:
-
intrusive or repetitive thoughts
-
compulsive or rigid behavior
-
internal restlessness
-
sensory sensitivity
-
emotional intensity
-
mental fatigue
These symptoms of OCD tend to worsen under stress, sleep loss, or inflammation—conditions known to amplify glutamate signaling.
Natural Treatments for OCD That Reduce NMDA and Glutamate Activity
Below are research-supported interventions commonly used in functional care.
N-Acetylcysteine (NAC)
-
balances glutamate
-
improves antioxidant defenses
-
reduces oxidative stress driving NMDA activation
Magnesium
-
natural NMDA channel blocker
-
reduces neuronal hyperexcitability
Glycine
-
modulates NMDA function in a stabilizing way
Creatine (context dependent)
-
supports brain energy systems
-
especially beneficial when methylation is impaired
Low-dose Ketamine (clinical use only)
-
temporarily blocks NMDA receptors
-
resets hyperactive neural circuits
Ketogenic or Low-Glutamate Diet Approaches
-
lower glutamate production
-
improve GABA balance
-
reduce excitatory drive contributing to overactive brain OCD patterns
These strategies form the backbone of many natural treatments for OCD, especially when serotonin-based medications are ineffective.
Dietary Glutamates and OCD Sensitivity in an Overactive Brain
Dietary glutamates (broths, tomatoes, aged cheeses, MSG) do not normally cross the blood-brain barrier (BBB).
But sensitivity increases when the BBB becomes compromised by:
-
inflammation
-
high oxidative stress
-
gut permeability
-
undermethylation
-
chronic illness
In these states, glutamate-rich foods may worsen symptoms of OCD, headaches, anxiety, or sleep disruption.
Elimination and reintroduction trials often clarify sensitivity.
Testing That Helps Explain Symptoms of OCD and Glutamate Imbalance
Testing is valuable when symptoms suggest a biochemical driver. Priority assessments include:
Whole Blood Histamine
Marker of methylation status (correlates strongly with undermethylation + OCD).
Zinc / Copper / Ceruloplasmin
Copper excess increases excitatory tone and glutamate activity.
Magnesium & B6 Levels
Essential cofactors for neurotransmitter balance and antioxidant function.
Organic Acids
Identifies glutamate load, oxidative stress, mitochondrial strain.
The DD Methylation Pathway Panel: A Key Tool in Natural OCD Treatment
Many individuals with persistent OCD symptoms demonstrate patterns of undermethylation on the Doctor’s Data Methylation Pathway Panel.
Key findings often include:
-
elevated SAH
-
low SAM/SAH ratio
-
elevated methionine
-
low glutathione markers
-
increased oxidative stress indicators
These patterns directly promote:
-
NMDA receptor overactivity
-
excess glutamate signaling
-
emotional rigidity
-
repetitive thinking
-
high anxiety tone
For patients seeking natural treatments for OCD, this panel provides the clearest roadmap for nutrient-based interventions (SAMe support, B6, magnesium, zinc, NAC, and stabilizing dietary protocols).
Scientific Background: Glutamate, NMDA, and the Neurobiology of OCD
Understanding Glutamate and NMDA:
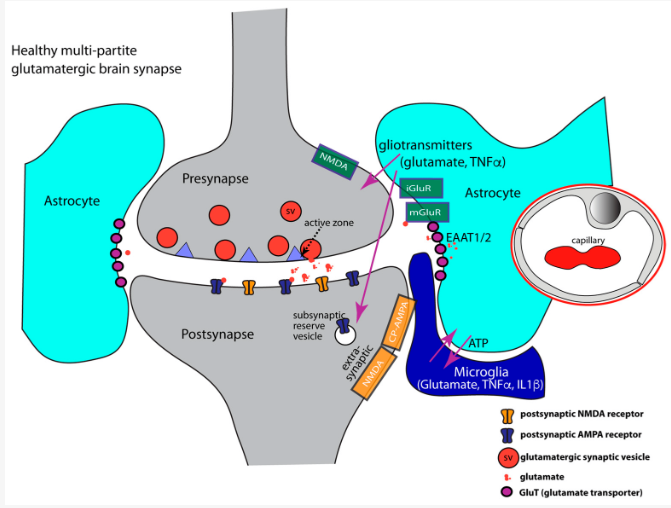
Glutamate is the brain's main "go" signal. When neurons communicate, they send messages to each other, and glutamate is a chief messenger that tells receiving neurons to activate or pass on a message. One primary way glutamate sends this message is by binding to specific proteins called receptors on neighboring neurons. The NMDA receptor is one such protein. Think of it as the traffic light at a busy city intersection, regulating the flow of cars or messages in the brain.
Receptors' Role and Why They Matter:
Receptors, like the NMDA receptor, are gatekeepers. They decide when and how strongly a neuron should react to messages like glutamate. Properly functioning receptors ensure our brain processes, from thoughts to emotions, run smoothly. However, if these receptors, or traffic lights, become overly active or malfunction, it's like letting too many cars through at once, leading to chaos and potential collisions. This overactivity can result in various challenges, including mood disorders, cognitive issues, and other neurological symptoms.
The Need to Regulate NMDA Activity:
Recent studies have shone a spotlight on NMDA receptors, linking their overactivity to a host of issues like anxiety, depression, and other mood disorders. As such, the idea is that by "turning down the volume" or down-regulating the activity of these receptors, we might alleviate some of these symptoms. It's akin to fine-tuning a radio to avoid static and get a clear signal. In the realm of mental health and neuroscience, understanding and potentially moderating NMDA receptor activity is becoming an increasingly promising area of exploration.
Methylation and NMDA Receptor Activity
- Histamine Levels: Undermethylation can lead to elevated histamine levels. Histamine, beyond its role in the immune response, is also a neurotransmitter. Elevated histamine can influence the excitability of neurons and enhance the activity of NMDA receptors. Some theories suggest that histamine may directly or indirectly enhance the influx of calcium through NMDA receptors, thus increasing their excitatory potential.
- Serotonin and Dopamine Activity: In undermethylators, there's an increased activity of serotonin and dopamine, not necessarily due to altered synthesis but primarily due to changes in their reuptake. The underlying mechanism is believed to be related to DNA histone overactivity, which leads to the excessive release of proteins (SERT and DERT) responsible for the reuptake of these neurotransmitters. As a result of this heightened reuptake protein expression from genes in neurotransmitter-producing cells, serotonin and dopamine remain active for shorter periods in the synaptic cleft. This reduced activity can indirectly influence the modulation and excitability of NMDA receptors, given the interconnected nature of neurotransmitter systems in the brain.
- Gene Expression Specificity: Methylation indeed regulates gene expression, but to be more specific, genes related to glutamate metabolism and regulation can be affected by methylation status. Changes in glutamate regulation directly impact NMDA receptor activity since glutamate is the primary neurotransmitter that activates these receptors. Altered gene expression might lead to an imbalance between excitatory and inhibitory signals, favoring overactivity at the NMDA receptors.
- Homocysteine Levels: While both overmethylation and undermethylation can influence homocysteine levels, in the context of undermethylation, elevated homocysteine can affect glutamate release and uptake, impacting the overall excitatory environment of the brain and potentially enhancing NMDA receptor activity.
Overactivity of NMDA receptors (NMDARs)
Overactivity of NMDA receptors (NMDARs) can result in a range of neurological and psychiatric consequences. The symptoms and problems associated with heightened NMDAR activity include:
- Excitotoxicity: Prolonged or excessive activation of NMDARs can lead to a phenomenon called excitotoxicity. This is where neurons become damaged and can die because of excessive stimulation. Excitotoxicity is implicated in various neurodegenerative diseases, including Alzheimer's disease, Parkinson's disease, and multiple sclerosis.
- Seizures: Overstimulation of NMDARs can heighten neural excitability, increasing the risk of seizures.
- Mood Disorders: Altered NMDAR activity has been implicated in certain mood disorders, including major depressive disorder and bipolar disorder.
- Psychotic Disorders: Abnormal NMDAR function is theorized to play a role in conditions like schizophrenia. Notably, drugs that block NMDARs, like phencyclidine (PCP) and ketamine, can induce psychotic symptoms in healthy individuals, further suggesting a connection.
- Cognitive Impairment: Overactivity of NMDARs can disrupt neural circuits related to cognition, leading to issues like memory problems, difficulty concentrating, and other cognitive deficits.
- Anxiety: Some studies suggest that altered NMDAR function might play a role in anxiety disorders.
- Chronic Pain: NMDARs are involved in pain perception, especially in the spinal cord. Their overactivity can contribute to certain chronic pain syndromes.
- Neurodevelopmental Disorders: Abnormal NMDAR signaling during critical developmental periods might be associated with disorders like autism spectrum disorder and ADHD.
- Sleep Disruptions: Given the broad role of NMDARs in neural processing, they can influence sleep patterns, potentially leading to insomnia or other sleep disturbances when overactive.
- Oxidative Stress: Excessive NMDAR activity can increase the production of reactive oxygen species, contributing to oxidative stress, which can damage cells.
- Increased Calcium Influx: Overactive NMDARs can allow excessive calcium to enter neurons. This can disrupt cellular processes, potentially leading to cell death.
How Glutamates in Food Affect NMDA Receptors
Dietary glutamates matter far more for individuals with NMDA-related sensitivity, OCD, anxiety, mold exposure, or undermethylation than for the general population.
In healthy physiology, the blood–brain barrier limits glutamate entry. But many patients with neuroinflammation, high histamine, copper overload, mold-related injury, mast-cell activation, or oxidative stress have a more permeable BBB and impaired glutamate clearance. In these states, foods high in glutamate—MSG, broths, tomatoes, aged cheeses, protein isolates—can intensify NMDA receptor activation, increasing anxiety, intrusive thoughts, overstimulation, headaches, or insomnia.
The gut and liver normally metabolize dietary glutamate, but when inflammation, dysbiosis, or mitochondrial inefficiency is present, even modest exposures may trigger symptoms. This explains why some individuals feel dramatically worse after restaurant meals or processed foods while others experience no effect at all.
In short, dietary glutamate is not universally harmful, but for those with NMDA hyperexcitability or impaired biochemical regulation, reducing glutamate-rich foods often provides meaningful symptom relief.
Obsessive-Compulsive Disorder (OCD) and NMDAR
OCD is characterized by persistent and unwanted thoughts (obsessions) and repetitive behaviors or mental acts (compulsions). The exact neurobiological mechanisms underlying OCD are not fully understood, but the involvement of the glutamatergic system, and in particular the NMDA receptors (NMDARs), has gained significant attention.
Here's why the role of NMDARs and potential intervention with N-acetylcysteine (NAC) is relevant to OCD:
- Glutamatergic Dysregulation: Neuroimaging and cerebrospinal fluid studies have shown alterations in glutamate levels in certain brain regions, like the basal ganglia and the anterior cingulate cortex, in individuals with OCD. Overactivity of the glutamatergic system might contribute to the heightened neural circuit activity observed in OCD.
- Cortico-Striato-Thalamo-Cortical (CSTC) Loop: This is a neural circuitry loop that involves parts of the cortex, the striatum, and the thalamus. Disruptions or overactivity in this loop has been implicated in OCD. Given the role of glutamate as the primary excitatory neurotransmitter, it's hypothesized that NMDAR hyperactivity might contribute to the hyperactivity of the CSTC loop, leading to persistent thoughts and repetitive behaviors.
- NAC's Role: NAC, as previously mentioned, modulates glutamate levels and activity in the brain. By regulating the release and reuptake of glutamate, NAC might help balance the glutamatergic system and, in turn, modulate the overactive neural circuits associated with OCD.
- Neuroprotection and Synaptic Plasticity: Beyond its modulation of glutamate, NAC has antioxidant and neuroprotective properties, which can aid in protecting neurons from potential damage (like that which could arise from excessive glutamatergic activity). NAC might also influence synaptic plasticity, which is the ability of synapses to strengthen or weaken over time. This can be relevant in disorders like OCD where certain neural pathways may have become excessively reinforced.
- Other Neurotransmitter Systems: OCD is multifactorial, and other neurotransmitters like serotonin play significant roles. NAC, given its broad effects, might also have indirect effects on other neurotransmitter systems, contributing to its potential therapeutic benefit.
For sufferers of OCD, the recurring loop of thoughts and behaviors can be mentally exhausting, affecting their daily life, relationships, and overall well-being. The implication of NMDARs and the potential for interventions like NAC offer hope for more targeted and effective treatments. If NAC can modulate the overactive neural circuits and neurotransmitter imbalances underlying OCD, it might reduce the intensity and frequency of obsessions and compulsions, providing relief for those affected by the disorder.
Other Symptoms Associated with Excess NMDAR Activity
NMDAR excitotoxicity refers to the damage and death of neurons due to excessive stimulation by neurotransmitters, such as glutamate, acting on NMDA-type receptors. When NMDA receptors are overly stimulated, they allow too much calcium (Ca^2+) into cells, which can then activate enzymes that damage cell structures. This process is implicated in various acute and chronic neurological disorders. Here are some of the physical, emotional, and cognitive symptoms associated with NMDAR excitotoxicity:
Physical Symptoms:
- Seizures: Excessive excitatory activity can lead to uncontrolled neural firing patterns.
- Motor Dysfunction: Issues like spasticity, rigidity, or weakness can arise.
- Pain: Particularly neuropathic pain or pain syndromes associated with central sensitization.
- Hearing Loss: Especially if the excitotoxicity affects the auditory nerve.
- Visual Problems: Such as loss of vision or disturbances if the optic nerve or related pathways are affected.
- Respiratory Issues: Breathing problems might emerge if excitotoxicity affects areas of the brain responsible for respiratory control.
Emotional/Cognitive Symptoms:
- Mood Disorders: Including depression and bipolar disorder.
- Anxiety: Heightened or excessive worry and stress.
- Psychotic Symptoms: Such as hallucinations and delusions. Drugs that block NMDARs, like PCP and ketamine, can induce psychotic symptoms in healthy individuals.
- Memory Issues: Especially problems with short-term memory or memory consolidation.
- Difficulty Concentrating: Or other cognitive deficits.
- Behavioral Changes: Such as irritability, aggressiveness, or apathy.
Other Symptoms:
- Sleep Disturbances: Insomnia, disrupted sleep patterns, or excessive sleepiness.
- Headaches or Migraines: Due to altered neural activity or changes in cerebral blood flow.
It's important to note that NMDAR excitotoxicity is just one potential factor among many in the development of these symptoms. Additionally, while excitotoxicity can contribute to these issues, not everyone experiencing NMDAR excitotoxicity will manifest all, or even any, of these symptoms. The presentation largely depends on which specific neural pathways or areas of the brain are most affected.
Promising Therapies in Glutamate Modulation
N-ACETYLCYSTEINE (NAC) - NAC is a versatile compound with a range of proposed neuroprotective and neuromodulatory effects. Dr. William Walsh's "Walsh Approach" highlights the use of nutrients, like NAC, in the treatment of mood disorders and other neuropsychiatric conditions. Here's how NAC might influence NMDAR function and address some of the related issues:
-
- Antioxidant and Neuroprotection: One of NAC's primary roles is serving as a precursor to glutathione, a potent intracellular antioxidant. By boosting glutathione levels, NAC can counteract oxidative stress, a potential consequence of overactive NMDARs. This might offer protection against excitotoxicity, a damaging effect of excessive NMDAR activity.
- Modulation of Glutamate: NAC can modulate glutamatergic systems, which directly impact NMDAR function. Specifically, NAC might regulate the release and reuptake of glutamate, which in turn can influence NMDAR activation.
- Homocysteine Metabolism: Elevated levels of homocysteine can increase the excitatory tone in the brain, potentially promoting NMDAR overactivity. By facilitating the conversion of homocysteine to cysteine (which can then be used for glutathione synthesis), NAC might help maintain a balanced excitatory environment.
- Methylation Pathway: As you pointed out, an accumulation of homocysteine can lead to an increase in S-adenosylhomocysteine (SAH), which inhibits methylation reactions. By aiding in the metabolism of homocysteine, NAC can potentially relieve this bottleneck and support healthy methylation processes.
- Anti-inflammatory Effects: Chronic inflammation can exacerbate or contribute to many neurological and psychiatric conditions. NAC has anti-inflammatory properties which, while not directly related to NMDAR function, can be beneficial in a broader sense for neural health.
- Neurogenesis: There's some evidence to suggest that NAC can promote neurogenesis (the formation of new neurons) in certain parts of the brain. While this isn't a direct modulation of NMDARs, enhancing neurogenesis could be beneficial for overall brain function and resilience.
KETAMINE ((RS)-2-(2-Chlorophenyl)-2-(methylamino)cyclohexanone) - an anesthetic in large doses, it can produce profound dissociative effects. At these doses, it acts primarily as an antagonist of the NMDA receptor, meaning it blocks the receptor's function. However, when used in lower doses, such as in the microdosing context or in subanesthetic doses for the treatment of conditions like depression, its mechanism of action becomes more multifaceted and intriguing. Here's how microdosing or low doses of ketamine might help with NMDAR excitotoxicity and other neural dysfunctions:
-
- NMDA Receptor Blockade: Even at lower doses, ketamine still acts as an NMDA receptor antagonist. By temporarily blocking these receptors, ketamine can reduce excitatory signaling, potentially offering protection against excitotoxicity. The transient reduction in excitatory signaling can essentially "reset" certain neural pathways, which might contribute to its rapid antidepressant effects.
- Synaptic Plasticity: One of the most discussed effects of low-dose ketamine is its ability to rapidly enhance synaptic plasticity. It promotes the growth and formation of new synapses in certain brain regions, particularly the prefrontal cortex. This is believed to be one of the main mechanisms behind ketamine's rapid antidepressant effects.
- Indirect Effects on Other Neurotransmitters: While NMDA receptor blockade is ketamine's primary action, it has secondary effects on other neurotransmitter systems. For instance, ketamine can increase the release of glutamate in certain brain regions. This might sound counterintuitive given its role as an NMDA receptor blocker, but this increased glutamate release can activate other types of glutamate receptors (like AMPA receptors) that play roles in synaptic plasticity and mood regulation.
- Neurotrophic Factors: Ketamine has been shown to increase the levels of brain-derived neurotrophic factor (BDNF). BDNF is essential for the survival and growth of neurons and the formation of new synapses. This effect might contribute to ketamine's ability to rapidly enhance mood in people with depression.
- Anti-inflammatory Effects: Some studies suggest that ketamine has anti-inflammatory effects in the brain, which might contribute to its neuroprotective and mood-enhancing properties.
Regarding the comparison to its anesthetic effects: While ketamine's action as an NMDA receptor blocker is consistent across doses, the overall experience and the broader physiological effects differ between anesthetic and low doses. Anesthetic doses aim to produce profound dissociation and loss of consciousness, while low doses might produce mild changes in perception and cognition without significant dissociation.
While the blockade of NMDA receptors plays a role in ketamine's effects at low doses, its therapeutic benefits in conditions like depression seem to arise from a combination of enhanced synaptic plasticity, modulation of other neurotransmitter systems, increased neurotrophic factors, and potential anti-inflammatory effects.
Other NMDA Receptor Antagonists and Neuroprotective Supplements
A number of other supplements have been studied for their potential role in modulating NMDA receptor activity and reducing inflammation. Here are some of the most notable:
- Magnesium: Magnesium acts as a natural NMDA receptor antagonist. When present in sufficient amounts, it can block the channel of the receptor, preventing excessive calcium influx and thus protecting against excitotoxicity. Magnesium deficiency can increase the risk of NMDA receptor hyperactivity.
- Omega-3 Fatty Acids: These have anti-inflammatory properties and are essential for maintaining the health of neuronal membranes. EPA and DHA, two primary omega-3 fatty acids found in fish oil, have been shown to be neuroprotective and may modulate NMDA receptor activity.
- Vitamin D: It has a role in regulating calcium in neurons and can affect NMDA receptor function. Low vitamin D levels have been associated with several neurological conditions.
- Zinc: Zinc can modulate the function of NMDA receptors, acting in a somewhat similar manner to magnesium. However, its interaction with the receptor is more complex and depends on its concentration.
- Curcumin: Found in turmeric, curcumin has potent anti-inflammatory properties and has shown neuroprotective effects in some studies. It might influence glutamate levels and NMDA receptor activity.
- L-Theanine: An amino acid found primarily in tea leaves, L-theanine has been suggested to modulate NMDA receptor activity and promote a calming effect on the brain.
- Taurine: An amino acid that can act as an inhibitory neurotransmitter, taurine has been shown to modulate NMDA receptor activity in some studies.
- Bacopa Monnieri: Traditionally used in Ayurvedic medicine, this herb might have neuroprotective properties and has been investigated for its potential to modulate NMDA receptor activity.
- Ginkgo Biloba: This ancient plant extract has potential neuroprotective properties, possibly due to its antioxidant action and ability to modulate neurotransmitter systems, including the glutamatergic system.
- B Vitamins: Particularly B6, B9 (folate), and B12, these vitamins are critical for homocysteine metabolism. Elevated homocysteine has been implicated in various neurological disorders and can potentially affect NMDA receptor activity.
It's essential to approach the use of supplements with caution. While they can offer therapeutic potential, it's crucial to consult with healthcare professionals before starting any supplementation, especially when aiming to address specific medical conditions or symptoms. The doses, interactions with other medications or supplements, and potential side effects need to be considered.



