Copper Overload Symptoms — Updated Science on Neurotransmitters, Ceruloplasmin & Walsh Theory
Copper overload symptoms are increasingly recognized as a major cause of anxiety, agitation, sensory overwhelm, panic, mood swings, irritability, and neurochemical instability. For many patients, these symptoms appear without a clear psychological trigger. Modern research now shows that copper excess does not simply raise serum values — it alters neurotransmitter activity, affects DBH-containing vesicles, elevates norepinephrine activity, amplifies glutamate/NMDA signaling, reduces GABA tone, and increases oxidative stress in the brain.
This expanded understanding also reflects Dr. William Walsh’s most current explanation: copper overload increases norepinephrine activity not because DBH “speeds up,” but because copper alters synaptic handling, storage, and release of neurotransmitters — especially catecholamines — while simultaneously increasing excitatory signaling and oxidative stress.
Together, these mechanisms explain why individuals with anxiety, autism traits, postpartum changes, pyroluria, undermethylation, or hormonal fluctuations often experience significant emotional symptoms when copper rises.
Understanding Copper Overload Symptoms Through Modern Neurochemistry
Copper overload symptoms go far beyond headaches, nausea, or metallic taste. In the nervous system, elevated copper modifies neurotransmitter pathways that regulate stress tolerance, mood stability, sensory processing, and cognitive flexibility. The most consistent features include:
-
Heightened anxiety or panic
-
Irritability and emotional lability
-
Racing thoughts or agitation
-
Insomnia and overstimulation
-
Stress intolerance and noise sensitivity
-
Tension, muscle tightness, or restlessness
-
Flushing, dizziness, or nausea when copper mobilizes (“dumping”)
These symptoms arise because copper influences dopamine, norepinephrine, glutamate, and GABA — not through a single enzyme, but through interconnected biochemical pathways.
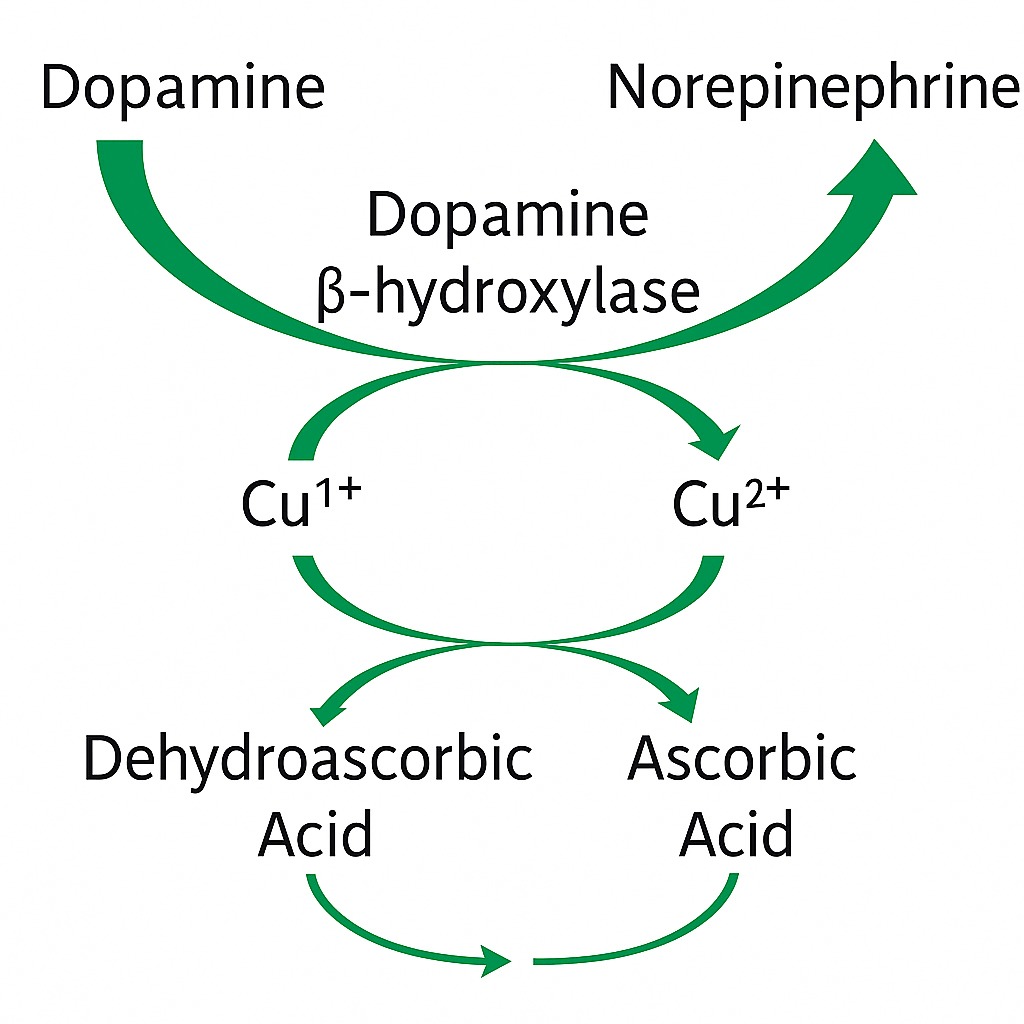
Copper, Dopamine β-Hydroxylase, and Norepinephrine: What Research Shows Now
Historically, clinicians believed high copper increased the speed of dopamine β-hydroxylase (DBH), converting dopamine into norepinephrine more rapidly. But biochemical research has clarified that:
✔ DBH becomes saturated at low copper levels
Adding more copper does not accelerate the enzyme. Multiple studies confirm that DBH activity plateaus once copper binding sites are filled.
✔ So why do high copper levels produce norepinephrine-dominant symptoms?
Modern findings — and Walsh’s updated model — show:
-
Copper alters vesicular storage and release of DBH, leading to abnormal norepinephrine output.
-
Copper disrupts synaptic regulation of catecholamines, increasing excitatory tone even without faster enzyme kinetics.
-
Oxidative stress generated by high copper degrades dopamine, lowering dopamine tone and shifting the catecholamine balance toward norepinephrine.
The result: high norepinephrine activity with low dopamine resilience — a pattern identical to the copper overload symptom cluster.
Glutamate, GABA, and NMDA: How Copper Creates Excitatory Dominance
Copper imbalance influences the excitatory–inhibitory balance of the brain:
1. Glutamate clearance decreases
High copper interferes with glutamate transporters, allowing glutamate to accumulate between neurons.
2. NMDA receptors become dysregulated
Copper modulation of NMDA receptors contributes to:
-
sensory hypersensitivity
-
anxiety
-
agitation
-
cognitive overload
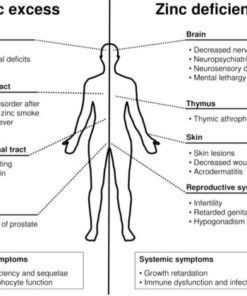
3. GABA activity weakens
Copper excess — and especially zinc deficiency — reduces GABA-A receptor function, weakening the calming side of the nervous system.
This triad creates overstimulation, a hallmark of copper overload symptoms.
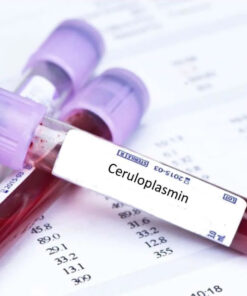
Why Ceruloplasmin Matters: Free Copper vs. Total Copper
Total copper does not tell the full story. Ceruloplasmin is the protein that binds and safely transports copper. When ceruloplasmin is low:
-
“Free copper” rises
-
Oxidative stress increases
-
Neurotransmitter imbalance worsens
-
Copper becomes more biologically reactive
Low ceruloplasmin appears in:
-
pyroluria
-
undermethylation
-
chronic stress
-
estrogen dominance
-
postpartum states
-
vegan/vegetarian diets low in zinc
-
inflammation
-
chronic infections
-
copper IUD use
This explains why many people develop copper overload symptoms even when total copper levels appear “normal.”
Causes of High Copper: Genetics, Hormones, Diet & Environment
Copper elevation usually arises from a combination of biological vulnerabilities and environmental exposure. Key contributors include:
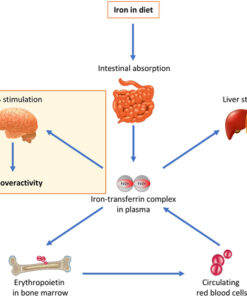
Low zinc
Zinc and copper compete for absorption. Low zinc increases copper retention and reduces metallothionein’s ability to bind and eliminate copper.
Pyroluria
High pyrroles deplete zinc and B6, leading to secondary copper excess.
Undermethylation
Reduces ceruloplasmin synthesis, increasing free copper.
Estrogen exposure
Oral contraceptives, IUDs, HRT, pregnancy, and postpartum shifts all raise copper.
Dietary factors
Vegetarian/vegan diets (high copper), chocolate, nuts, seeds, shellfish, organ meats.
Environmental copper sources
Well water, copper pipes, cookware, contaminated plumbing.
Inflammation & obesity
Impact ceruloplasmin metabolism and copper storage.
Rapid weight loss or zinc therapy
Mobilizes stored copper — a process known as copper dumping.
Symptoms of Copper Dumping: What Happens When Copper Mobilizes
Copper dumping occurs when copper stored in tissues begins moving into the bloodstream faster than the body can bind it. This happens during:
-
zinc therapy
-
significant weight loss
-
hormonal transitions
-
detoxification episodes
Common symptoms of copper dumping include:
-
sudden anxiety spikes
-
irritability or overwhelm
-
headaches or nausea
-
metallic taste
-
insomnia or vivid dreams
-
skin flushing
-
temporary worsening of mood
These reactions do not mean the body is becoming more toxic — they indicate that copper is being mobilized for elimination.
Updated Walsh Perspective: Why Copper Overload Raises Norepinephrine Activity
Dr. William Walsh has clarified that while copper overload is strongly associated with elevated norepinephrine activity, the mechanism is not increased DBH speed. Instead:
-
Copper affects storage and release of DBH-containing vesicles.
-
Copper alters synaptic function, influencing neurotransmitter dynamics.
-
Excess copper reduces SOD1/SOD3, increasing oxidative stress, which lowers dopamine tone.
-
Copper imbalance influences NMDA, GABA, and serotonin receptors, amplifying excitatory signaling.
Walsh emphasizes that patients with elevated copper reliably improve when copper is normalized through zinc, metallothionein support, antioxidant therapy, and ceruloplasmin enhancement.
Evidence-Based Copper Overload Therapy
An effective copper overload therapy plan addresses both the source of excess copper and the biochemical consequences:
Zinc therapy
Increases metallothionein, enabling copper binding and excretion; improves NMDA and GABA regulation.
P5P/B6
Supports neurotransmitter synthesis and reduces oxidative stress.
Antioxidants (Vitamin C, E, NAC, selenium)
Restore glutathione and reduce copper-induced ROS.
Ceruloplasmin support
Protein-rich diet, methylation support (SAMe or TMG when indicated), anti-inflammatory measures, stress reduction.
Address hormonal contributors
Evaluate estrogen exposure, IUDs, HRT, and postpartum physiology.
Diet modification
Reduce high-copper foods temporarily; increase zinc-rich animal proteins.
This multi-pathway approach mirrors both Walsh’s clinical success and modern research on copper’s wide neurochemical effects.
Begin an Assessment for Copper Overload Symptoms
If copper overload symptoms resonate — anxiety, irritability, overstimulation, insomnia, or copper dumping during zinc treatment — an evidence-based evaluation can clarify the biochemical pattern.
Testing options include:
-
Serum copper
-
Ceruloplasmin
-
Plasma zinc
-
Whole blood histamine (methylation status)
-
Pyrroles (pyroluria)
-
Comprehensive Walsh biotype assessment
Free pre-consultations available to determine whether copper overload, pyroluria, undermethylation, low zinc, or hormonal factors are contributing to chronic symptoms.